Global priority: mental health
- Global priority: mental health
- Executive summary
- 1. Motivation
- 2. How much do those with mental health disorders suffer?
- 3. Scale: how big is the global mental health burden?
- 4. Neglectedness: What is being done?
- 5. Depression and anxiety in LMICs: Are there (more) effective interventions?
- 5.1 Effective interventions exist
- 5.2 Addressing social determinants is essential
- 5.3 Prioritising child and adolescent mental health
- 5.4 Strategies exist for scaling-up delivery of interventions
- 5.5 Current cost-effectiveness estimates for interventions in LMICs are limited
- 5.6 Existing resources are largely spent on ineffective mental hospitals
- 6. Why aren’t people getting (the most) effective interventions? The role of stigma
- 7. What can be done?
- Concluding remarks
- Further reading
- References
- Appendix A: Disability weights used for mental health disorders in the GBD
Executive summary
This report investigates the global burden of mental illness. It sets out how big the problem is, how much spending it receives, and how those resources are allocated. It then focuses specifically on what can be done to reduce anxiety and depression in low-income countries—the assumption is that this is the part of the problem where additional resources would have the highest impact. It closes by outlining some promising donation options and career paths in the area, but does not attempt to evaluate which of these options are the most impactful, or to compare mental health to other possible global priorities—that requires further research, which HLI is undertaking regarding donations. We expect this report will be most useful for those considering putting their career or charitable donations towards improving global mental health and who therefore want to gain a better understanding of the nature of the problem and what could be done about it.
What’s the problem?
Mental illnesses are among the worst, if not the worst, of life’s common misfortunes. Depression and anxiety are associated with bigger reductions in life satisfaction than debt, divorce, unemployment, Parkinson’s, or Alzheimer’s. All over the world, those with mental illnesses suffer human rights abuses; these can be severe as being chained or caged.
Around one in every nine people lives with a diagnosable mental health disorder. These disorders are responsible for 5% of the global burden of disease, as measured in disability-adjusted life years (DALYs), and 15% of all years lived with disability. These figures are likely to be a substantial under-estimate for several reasons, for instance, that suicides and self-harm are not attributed to the burden of mental health disorders.
The vast majority of people living with mental health disorders, even in rich countries, do not receive treatment. The issue is even more acute in LICs, where mental health spending amounts to US$0.02 per person per year. In terms of development assistance, HIV receives 150 times more funding, per DALY lost to the problem, than mental and substance abuse disorders combined.
Effective interventions to improve mental health exist and can be deployed at scale. The 2016 Disease Control Priorities report noted a range of effective interventions for preventing or treating mental illnesses, and for promoting good mental health. Although there are few mental health specialists in low-income settings, one tried-and-tested way to scale-up interventions is ‘task-shifting’, where lay health workers provide therapy under the training and supervision of professionals.
While several treatments are deemed cost-effective (according to conventional standards in healthcare) the evidence-base for cost-effectiveness in low-income settings is limited. Not only are there few estimates of cost-effectiveness, these are mainly from high-income country contexts; almost no outcomes are measured in terms of subjective wellbeing.
Current mental health budgets could be spent more effectively. Around 80% of mental health spending in low- and middle-income countries (LMICs) goes towards psychiatric hospitals. Mental health experts argue that carefully moving to community-based care would lead to better outcomes, given fixed budgets. Further improvement could come from integrating mental health services within primary healthcare and increasing the (limited) access to cheap pharmaceutical treatments, such as antidepressants.
Stigma and misunderstanding are a major problem. These are commonplace among the general public, policymakers, and health professionals. This causes an unfortunate cycle: individuals are unwilling to seek treatment or may not even know treatment is possible; policymakers, faced with this lack of demand, prioritise other matters; as result, stigma and misunderstandings persist.
What can be done?
In light of the barriers and solutions identified from the literature, we suggest several broad avenues through which donors could fund useful work or individuals, through their careers, could undertake this work themselves. We do not attempt to prioritise between these, or between mental health and other problems; that was outside the scope of this project and is a topic for further work. We encourage interested readers to conduct their own, supplementary research.
Research
There are many potentially valuable research directions. Examples include: identifying root causes of mental illnesses; improving preventive interventions; advancing the scale-up of existing treatments; and developing new treatments or improving existing ones.
Intervention delivery
This refers to providing individuals with interventions that prevent or treat mental disorders or promote good mental health. This direct work could be carried out by funding, founding, or joining effective non-profit or for-profit organisations. Donation advice in this area is currently quite limited; the Happier Lives Institute is working to provide some in the near future (see section 7, particularly 7.2).
Policy and advocacy work
Mental health policy and advocacy work could raise public awareness of mental health disorders and press decision-makers, such as those in governments, to provide more and better services. This might include grassroots campaigning, journalism, lobbying, or work in think-tanks at a national or international level.
The global burden of mental illness is substantial and receives scant attention. Fortunately, there are a range of ways to make progress on this problem and help people to live happier lives. We expect that improving mental health could be among the most impactful options for donors and for individuals seeking to do good with their careers.
1. Motivation
Around the planet, people with mental illnesses experience immense suffering. Of course, they always have. What has begun to shift, in just the last couple of decades, is that this problem has started to get serious attention. The world’s citizens are beginning to wake up to the fact that this suffering is real, substantial, widespread, treatable and yet, barely treated.
For individuals considering high-impact careers, and donors considering how to do the most good with their resources, previous research has indicated mental health may well be a global priority and that the issue merits further investigation (Plant, 2016; 2018; Elizabeth, 2017; Founders Pledge, 2019). This report aims to build on that research, providing more detail both about the nature of the problem and what could be done about it. The report is limited in that it does not claim what the most cost-effective ways to improve mental health are, nor how they compare to other priorities.
This report proceeds as follows.
- Section two discusses some of the ways mental health disorders impact both those individuals who suffer from them and society more broadly.
- Section three considers the global scale of the problem and comments on how this may be underestimated for a variety of reasons.
- Section four remarks on how neglected mental health is compared to physical health, how resources are currently allocated in mental health, and on the large treatment gap.
Sections five to seven consider what can be done to make progress, focusing specifically on ‘mood disorders’ – depression and anxiety – in low- and middle-income countries (LMICs). This restriction on scope was motivated by the expectation that these will be the problems, and the location, where the most cost-effective ways to increase wellbeing by reducing mental illness will be found.
- Section five notes there are some effective interventions and these could be provided at scale.
- Section six explains the importance of stigma in why these interventions aren’t being more widely used now.
- Section seven draws on the preceding analysis to say which actions private individuals or organisations might take to decrease the global burden.
- Section eight concludes.
Before going further, we should note some of what follows is presented in terms of mental, neurological, and substance use (MNS) disorders rather than mental health disorders. ‘MNS’ refers to a wide range of brain-related conditions including depression, epilepsy, and alcohol abuse. We do this because, in medicine, MNS are often grouped together and it has sometimes not been feasible for us to disentangle various statistics only to remark on the mental health aspect.1Although this report focuses on mental health disorders, future research into how individuals and organisations can use their resources to do the most good may wish to consider MNS disorders as a whole. There are several reasons for this: (a) drawing a clear distinction between mental, neurological, and substance use disorders from the literature is not always achievable; (b) MNS disorders share several risk factors and symptom characteristics (Patel et al., 2016a); (c) there is a high comorbidity among MNS disorders, meaning that multiple disorders are often experienced by a single individual (Patel et al., 2016a; Plana-Ripoll et al., 2019), for example, there is a high prevalence of mental health disorders among people living with substance use disorders (Shantna et al., 2009; NIDA, 2018); (d) social determinants affect both the risk and symptom expression of multiple MNS disorders (Patel et al., 2016a); (e) experiences of stigma and discrimination are common (Patel et al., 2016a); (f) MNS disorders are commonly chronic and relapsing (Patel et al., 2016a); (g) at the level of health systems in LMICs, MNS disorders are often said to be a single group, with the separation of MNS disorders largely being an invention of Western psychiatry (Whiteford et al., 2015; Vigo, Thornicroft and Atun, 2016), although this may not be clear cut (Patel et al., 2016a); and (h) in LMICs, MNS disorders are often designated a single shared budget (WHO Substance use disorders Atlas 2010).
2. How much do those with mental health disorders suffer?
Before considering the problem from a global perspective, we should focus on the individual experiences of those who suffer from mental health disorders; for the most part, sufferers receive no treatment (Wang et al., 2007; WHO Mental Health Atlas 2017). Despite the binary approach used for diagnosis, there is a wide diversity in these experiences, with symptoms and disorders existing across a spectrum from mild and short-lived distress, to chronic and severe conditions (Patel et al., 2018). This section will outline the impact of mental health disorders on subjective wellbeing (‘SWB’; self-reported measures of happiness and life satisfaction), human rights, individuals’ economic and social situations, and physical health.2SWB refers to individuals’ self-reported rating of how they feel about and during their lives (Stone and Mackie, 2013).
2.1 Mental health disorders and subjective wellbeing
A first question to ask is: how bad are mental health disorders for those that experience them? We assume that readers will, by now, have heard a range of first-hand qualitative accounts of what it is like to experience various mental illnesses: it has become refreshingly common for sufferers, including famous celebrities, to open up and tell their stories. Therefore, what we will do instead is try to quantify their badness and put it in context.
Data from a recent report by the Happiness Research Institute showed the correlation between 16 different health conditions and life satisfaction in a panel of Europeans over 45 years old (Happiness Research Institute, 2020). Depression and anxiety were, on average, associated with the largest per-person reductions in self-reported life satisfaction – greater than stroke, arthritis or lung disease (see figure 1). In fact, the reduction in life satisfaction associated with depression was about twice that of being unemployed, and three times the impact of being divorced compared to married. Symptoms of physical discomfort and mobility were much less predictive of life satisfaction than mental symptoms, such as loneliness, depression and anxiety, or optimism. Depression and anxiety are among the worst, if not the worst, of life’s common misfortunes.
Life satisfaction data from other high-income countries (HICs) such as the US and Australia, show mental health disorders to be associated with similarly large reductions in life satisfaction (World Happiness Report, 2017). In Indonesia, an upper-middle income country, mental health is more important than unemployment or years of education for predicting life satisfaction, although less important than income (World Happiness Report, 2017).
Why is this the case? Let’s consider some of the factors that cause and compound inner emotional turmoil.
Figure 1: Depression and anxiety are associated with large reductions in life satisfaction
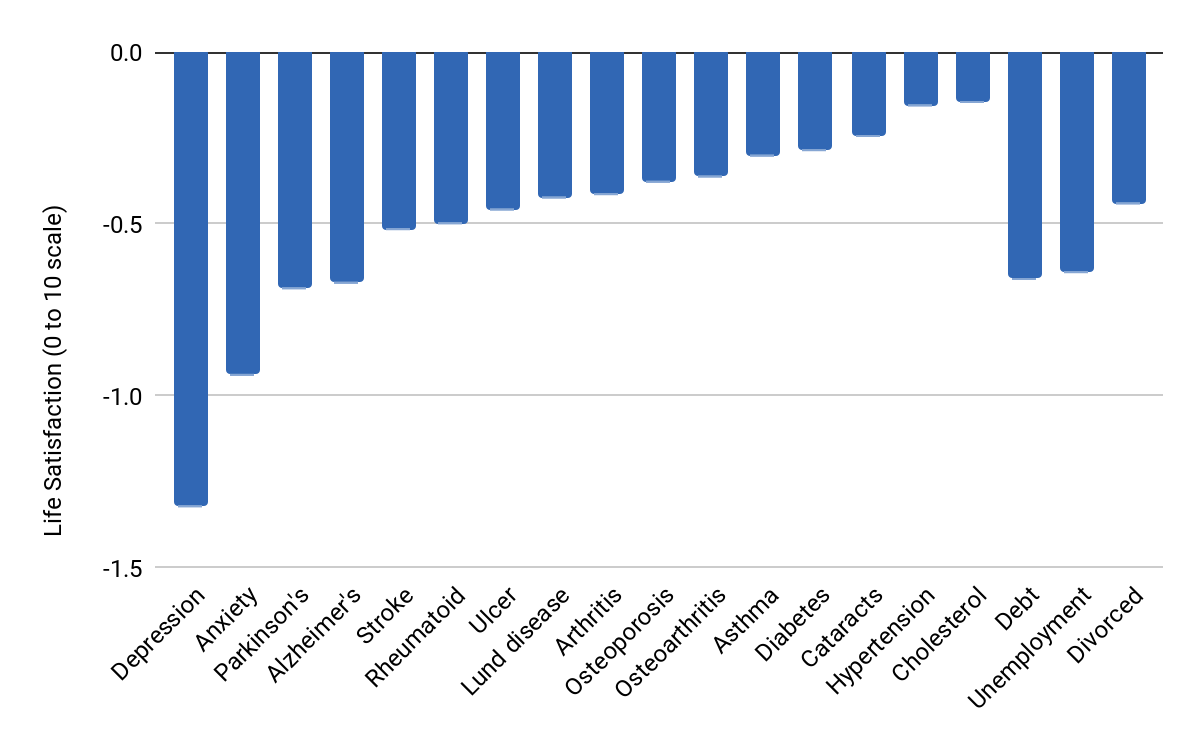
Note: Column chart showing the difference in life satisfaction between individuals living with 16 disorders and healthy counterparts. Figure adapted from Happiness Research Institute, 2020.
2.2 Human rights consequences
Having a mental health disorder can lead to human rights abuses, particularly for those who live with severe mental disorders such as schizophrenia and bipolar disorder. Abuses include being tied to beds or kept in isolation by family members or hospital staff, incarcerated in prisons, or being chained and caged within the community (Patel and Saxena, 2014, Human Rights Watch, 2016). Often, no consent from the individual or involvement of the judicial system is needed prior to this confinement (Human Rights Watch, 2016). People can be kept in these conditions for many years (Human Rights Watch, 2016), and it happens across many countries (Global Citizen, 2017; Independent, 2020; BBC, 2013a, Telegraph, 2019). As an extreme example, in Somalia, chains are said to be socially and medically accepted, and data collected in the country found that 90% of the treated patients had been constrained by chains at least once (WHO, 2010a). People living with mental health disorders also experience increased rates of homelessness and incarceration (WHO Report by the Secretariat, 2012). See Dudley et al. (2012) for a collection of articles on issues at the intersection of mental illness and human rights.
See Box 1 for a description of a recent Guardian article about life for those with mental disorders in Ghana, a country of 30 million people but only 13 psychiatrists (The Guardian, 2020).
|
Box 1: Selected quotes from ‘All we can offer is the chain’, The Guardian, 3 February 2020 Under the baobab tree two goats are tethered to the great trunk by ropes. Baba Agunga, a man in his twenties, is held by chains. A bracelet shackle round each of his ankles leads to a chain rusted to the same tone as the Ghanaian mud and welded tight around a thick, solid tree root. He sits naked on a cloth, hugging thin legs, his skin dusty dry and his eyes vacant. He has been there for three years says his mother, Aniah Agunga. Through winter and summer, rainy seasons and drought, he has been tethered outside the main compound of the village of Zorko, northern Ghana, within sight of the family hut. His father who put on the chains has since died, his two sisters have married, moved away, had children. All the while Baba Agunga hasn’t moved beyond the earthen circle allowed by his four feet of chain […] John Yimbilbe has been chained to a tree at Nyinbonya for two years, his wife Elizabeth Kwamwe says. She stays with him, the pair sitting side by side, lowering a mosquito net down from the tree at night to cover them. The pastor feeds them every day, but they would like the chains removed. Yimbilbe rattles his leg chains with one hand: “I hate them. I want to go home.” Kwamwe says he lost his job due to his “sadness” and would wander about at night so he was chained. “It comes into my mind sometimes to leave him, but he is my husband to take care of. There is love,” she smiles. |
2.3 Economic consequences
For a variety of reasons, such as lowered ability to work, distorted beliefs, and health expenditure, individuals living with mental health disorders are also more likely to face financial hardship (Ridley et al., 2020). Out-of-pocket payments are a common way of financing treatment, as mental health disorders are often excluded from insurance schemes (Chisholm et al., 2016a). People living with mental disorders are also excluded from disability benefit schemes in many LICs (Saxena et al., 2006). Mental illness is associated with the highest rates of unemployment of all disabilities globally (WHO Report by the Secretariat, 2012). It is also more difficult for family members of a person with a mental health disorder to find a new job, or hold onto an existing one (WHO, 2003). Ridley and colleagues outline multiple potential mechanisms through which mental disorders can cause or exacerbate poverty, as well as mechanisms through which poverty can cause mental illness (Ridley et al., 2020). The recurrent nature of mental disorders, their emergence during adolescence and impact on working age groups, as well as their intergenerational effects are all other important mechanisms leading to economic consequences (Ridley et al., 2020).
2.4 Social consequences
Living with a mental health disorder can also affect an individual’s relationships with others. Stigma, discrimination, and violence towards people living with mental health disorders and their families is common (WHO and UNDP, 2019). For example, research by the UK’s Time to Change campaign found that 9 out of 10 people using mental health services in England have experienced stigma and discrimination in their lives due to their mental health problems (Time to Change, 2008). Stigma may lead to anger, fear, avoidance, or self-discrimination, each of which can manifest in multiple ways throughout a person’s life (Corrigan and Watson, 2002). Stigma can make many aspects of an individual’s life harder. For example, a person living with a mental health disorder may be prevented from marrying into other families and in some cultures there is a belief that they bring shame to the family (Rasmussen et al., 2019).
2.5 Physical health consequences
There is a complex and bidirectional relationship between mental disorders and non-communicable physical diseases (Stein et al., 2019; WHO Report by the Secretariat, 2012). People living with psychosis, bipolar mood disorder, and moderate-severe depression have a reduction in life expectancy of 10-25 years (World Psychiatry. 2017) and the majority of these deaths are due to chronic physical health conditions (WHO, n.d.-b). There are a variety of risk factors contributing to this high excess mortality among persons with severe mental disorders (WHO, 2015a). Firstly, at the individual level, risk factors include lower engagement with the healthcare system and increased risk behaviours; secondly, at the health system level, persons with severe mental disorders often receive a poor quality of care for physical health conditions; and finally, at the level of social determinants of health, persons with severe mental disorders experience, for example, a greater likelihood of living in a less safe neighbourhood, fewer opportunities to engage in healthy activities, and are more likely to be socially isolated (World Psychiatry. 2017). Mental disorders are also likely linked to immune dysregulation (Bilbo and Schwarz, 2012), and people living with mental disorders have higher rates of infectious diseases (World Psychiatry. 2017).
3. Scale: how big is the global mental health burden?
This section explores the global burden of mental health disorders, including the health, economic and social costs. The disability burden of mental health disorders is comparable in scale to that of many physical health priorities; there are reasons to believe this burden is an underestimate.
3.1 The burden of mental health disorders is comparable to many physical health priorities
The Global Burden of Disease (GBD) project quantifies health loss from hundreds of diseases, injuries and risk factors (IHME, n.d.) and is the most comprehensive dataset measuring the burden of mental health disorders globally. Input data is collected from many sources, including administrative records, censuses, clinical trials, disease registries, surveys, and vital registration (IHME, 2020). In some countries, data are sparse (Leach-Kemon et al., 2013) and experts may have different opinions about the total figure for all-cause mortality (IHME, 2020). Data are also more commonly missing from countries with fewer resources (Leach-Kemon et al., 2013).
Figure 2: Mental health disorders were responsible for 4.9% of all DALYs in 2019
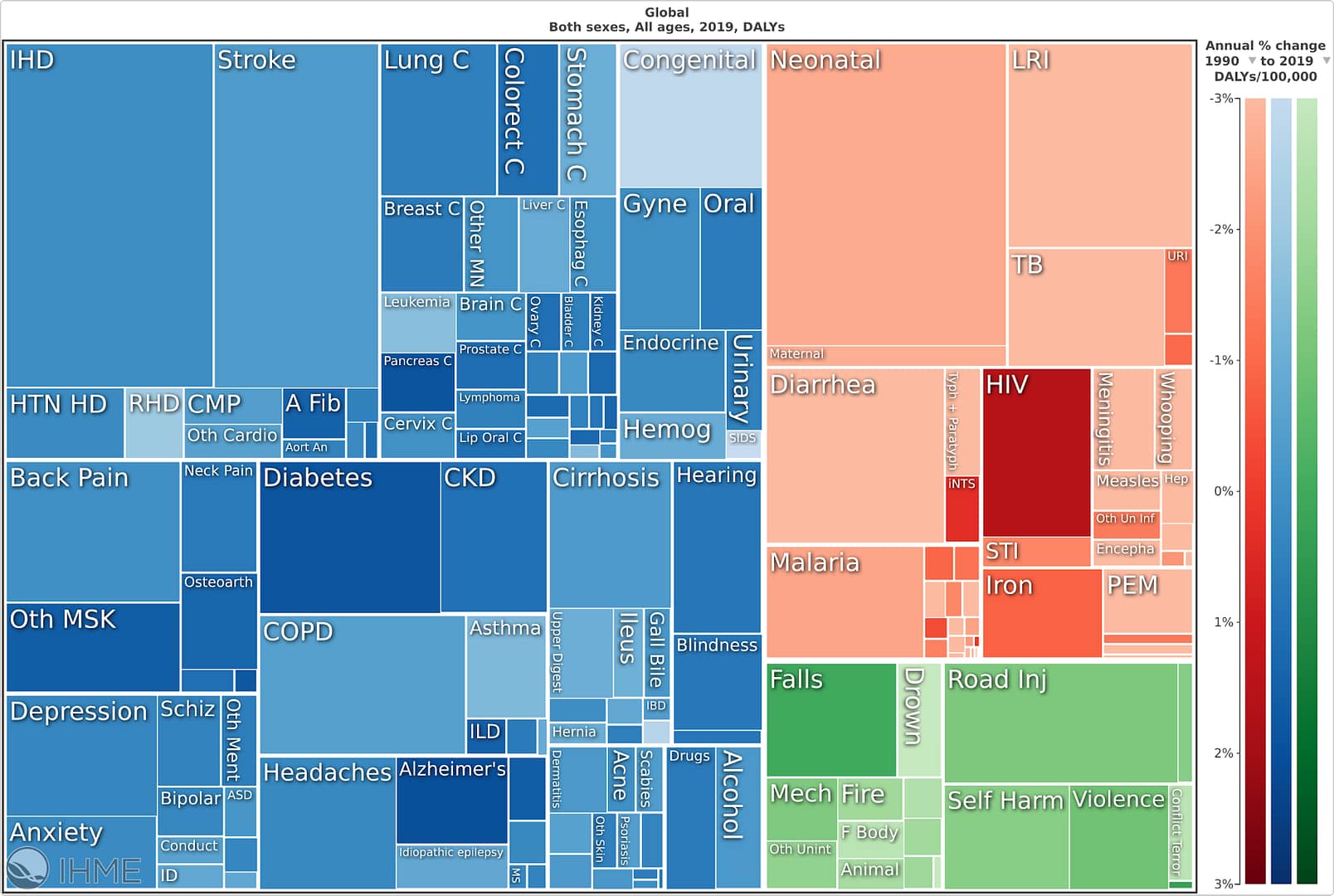
Note: This square pie chart shows the proportion of DALYs attributed to every cause of disability and death included in the Global Burden of Disease study in 2019. The area of each box is proportionate to the number of DALYs attributed to this cause. Non-communicable diseases are shown as blue boxes; communicable, maternal, neonatal and nutritional disorders are shown as red boxes; and injuries are shown as green boxes. A darker shade of colour is used to indicate a percentage increase in the number of DALYs caused by a given disorder from 1990 to 2019, whereas paler shades indicate a percentage decrease. Figure from IHME Viz Hub, n.d.
The GBD estimates that 792 million people were living with a mental health disorder in 2017 (10.7% of the world’s population) (Our World in Data). The two highest-prevalence mental disorders were anxiety and depression, experienced by 3.8% and 3.4% of the global population, respectively.
In addition to the prevalence, it is useful to consider deaths and disability caused by mental health disorders. DALYs are made up of both years lived with disability (YLDs) and years of life lost (YLLs). Mental health disorders made up 4.9% of DALYs globally in 2019, but 14.6% of YLDs globally. Mental health disorders, with the exception of eating disorders, are assumed not to cause any deaths, something we discuss in the next section as contributing to their under-estimation (see figure 2) (GBD, n.d.). The proportion of DALYs caused by mental health disorders is higher in HICs than in LMICs, partly due to the greater burden of other health conditions in LMICs (GBD, n.d.; Patel et al., 2016b). In addition, 17 of 18 mental disorders are estimated to have a higher prevalence in HICs than in LMICs (Scott et al., 2018).3The low prevalence of mental disorders in LMICs is termed the vulnerability paradox (Mulder, Scott and Jorm, 2020). It seems difficult to explain in the face of highly prevalent mental health risk factors in lower income countries (Cahill and Romei, 2019; Plan International, 2012). For example, in sub-Saharan Africa, 36% of the population are affected by intimate partner violence (McCloskey et al., 2016), 43 million children have lost one or both parents (Stover et al., 2007), rates of sexual violence are high (Cahill and Romei, 2019), and physical punishment is still allowed by teachers in 77 countries (Plan International, 2012). There are a wide variety of possible explanations for this paradox, including methodological problems, stigma and cultural factors causing underreporting, or the presence of factors which promote mental health in LMICs, such as greater community engagement (Mulder, Scott and Jorm., 2020). Alternatively, there is a hypothesis that depression is a disease of modernity (Hidaka, 2012). Suggested reasons why this could be the case include differences in diet, exercise, light, sleep, and cultures, such as differences in emphasis on individualism (Hidaka, 2012). The absolute number of DALYs in LMICs is still higher than that in HICs, due to the larger population size of LMICs (Patel et al., 2016b). Particularly large contributors to the DALY burden in LMICs are depression and anxiety (see figure 3) (GBD, n.d.).
Overall, the number of DALYs caused by mental health disorders increased by 55% from 1990 to 2019, although the prevalence of mental health disorders increased by only 1% over this time period (GBD, n.d.); in other words, the numbers have gone up due to population increases, rather than issues becoming more or less common per person. It is possible demographic changes, income inequality, and climate change will cause the burden of mental health disorders to rise (Patel et al., 2018; Lund et al., 2018; Lund, 2019). The percentage of DALYs caused by mental health disorders is increasing in both lower-middle income countries and low income countries (GBD, n.d.), partially due to the falling burden of DALYs caused by physical health problems such as communicable, maternal, neonatal and nutritional deficiencies (GBD, n.d.).
The high prevalence of mental health disorders in areas affected by conflict, disasters and other emergencies is noteworthy. For example, more than one in five people at any one time in post-conflict settings are estimated to have a mental disorder (Charlson et al., 2019). YLDs caused by depression and post-traumatic stress disorder in conflict-affected settings are estimated to be five times greater than the global mean estimates (Charlson et al., 2019). There is reason to expect the COVID-19 pandemic to increase the burden of mental disorders and further research will be necessary in order to better understand these effects (Vigo et al., 2020; Maulik, Thornicroft and Saxena, 2020).
Figure 3: Mental health disorders were responsible for millions of DALYs in 2019

Note: Bar chart showing the number of DALYs (in millions) caused by mental health disorders in 2019, by World Bank income group. Data from GBD, n.d.
3.2 The global burden of mental health disorders is likely underestimated
The burden of DALYs, as recorded in the GBD, is a helpful guide for comparing the scale of different causes of death and disability globally. However, there are many reasons why the GBD likely underestimates the burden caused by mental health disorders. It is not straightforward to combine these and reestimate the number, but a doubling, or more, does not seem implausible.4 It is possible that experts in other disciplines believe their studied disorders are likewise underestimated; we have not carried out a comparative analysis.
Suicide and self-harm are classified in the GBD as injuries, meaning that none of the associated DALYs are attributed to mental health disorders. The percentage of suicides attributable to mental health disorders is estimated to be between 60% and 98% (Bachmann, 2018). As suicide accounts for nearly 800,000 deaths per year (WHO, 2017), Vigo, Thornicroft, and Atun (2016) argue that including suicide and self-harm would increase the DALY burden of mental health by 30%.
Diagnostic criteria for mental health disorders are Western and therefore may underestimate the prevalence of conditions in countries where the inhabitants understand such disorders differently (Whiteford et al., 2016). For example, some languages do not include words to describe the Western meaning of “sadness” or “depression” (Whiteford et al., 2016). In many LMICs, physical symptoms such as fatigue, aches, and pains may be the primary complaint for people with depression and anxiety rather than emotional symptoms (Hyman et al., 2016). Illustrating this problem, when psychiatrists familiar with the local cultural context in China asked follow-up questions for clarification, in addition to the standard Western diagnostic questions, the one-month prevalence of any mental disorder was found to be 17.5%, much higher than previous estimates that ranged from 1.1% to 9.1% (Phillips et al., 2009).5 Not Otherwise Specified (NOS) disorders were also included in the 17.5% figure; when these were excluded, the one-month prevalence was still 13.3%.
Mental disorders exist along a continuum (Caspi et al., 2014), but the GBD uses a binary diagnostic criterion, therefore not capturing mental illness which falls below the given threshold. A binary criterion seems far more suitable for physical disorders, where an individual without a given disorder can be assumed not to suffer from any relevant symptoms of that condition. Common symptoms such as anxiety and low mood are vastly more prevalent among populations than mental disorders meeting diagnostic criteria (Das-Munshi et al., 2008). Such subsyndromal symptoms actually account for a greater number of doctor’s visits and suicides than suprathreshold disorders (Rusico, 2019).
Relatedly, DALYs capture only the burden of mental disorders ignoring the value of good mental health (Shekhar Saxena, pers. comms., 2020). Clearly, there is an important difference between not being depressed and being happy. Counter-intuitively, then, an intervention that made mentally healthy people happier would avert zero DALYs.
Finally, DALYs likely underweight the badness of mental suffering compared to physical suffering. Disability weights are calculated based on answers to comparison questions posed to the general public regarding health states (Vos et al., 2016, supplementary material).6Each disorder in the global burden of disease is assigned a disability weight, which corresponds to the severity of a disorder. This can take any value between 0 and 1, where 0 reflects ideal health and 1 reflects death. Disability weights used for a variety of mental health disorders can be found in Appendix 1. However, there is relevant evidence suggesting that the public not only underestimate the effect anxiety and depression have on enjoyment of life and on the quality of relationships compared to the impact of physical problems (Karimi, Brazier and Paisley, 2017) but also rate depression significantly more favourably than depressed patients do themselves (Pyne et al., 2009). This is likely because it is more difficult to bring to mind the suffering caused by mental illness than the impacts of physical disability (Happiness Research Institute, 2020).
Also contributing to the scale of the mental health disorder burden, and not included within DALYs, are the economic costs which occur both on an individual level (as above) and on a societal level. The World Economic Forum’s investigation into the global economic burden of non-communicable diseases estimated mental illness to cost 3.8% of global GDP in 2010, and these costs can be expected to more than double by 2030 (Bloom et al., 2011).7This estimation includes direct personal medical and non-medical costs, and lost income due to mortality, disability and care seeking (Bloom et al., 2011).
When using DALYs to infer the total costs to society, Bloom et al., 2011 estimated that mental illnesses cause larger economic losses than other non-communicable diseases, such as cancer, cardiovascular disease, and diabetes. The societal economic costs of mental health disorders include: healthcare costs; lost opportunity costs; unemployment and welfare costs; productivity costs, including absenteeism and presenteeism (attending work but with reduced productivity); and high turnover of staff due to mental health reasons (Gorringe et al., 2020). Globally, the days of productivity lost due to mental illness are estimated to be worth more than one trillion dollars per year (Chisholm et al., 2016b). Although much of the literature on the economic costs of mental health focuses on HICs (World Bank and WHO, 2016), more than one third of the global costs are estimated to occur in LMICs (Bloom et al., 2011).
The consequences of mental health disorders on those around the affected individual must also be considered separately from the DALY burden. Family members are commonly the primary caregivers of people with mental health disorders (WHO, 2003; WHO, 2006). One survey found that nine out of ten adult respondents’ lives had been impacted by mental health challenges in some way, with 85% of workers being close to someone with experience of mental health difficulties (Accenture, 2018). Wider impacts, such as on children, are significant but rarely included in economic evaluations of treatment for mental health disorders (Knapp and Wong, 2020). For example, depression among mothers is associated with increased risk of depression among children, as well as higher rates of diarrhoeal and respiratory diseases, stunting, hospital admissions, and reduced immunisation (Goodman, 2020; WHO, Unicef and World Bank, 2018). About 15-23% of children live with a parent with a mental illness, predisposing them to a higher risk of mental disorders (Gorringe et al., 2020).
4. Neglectedness: What is being done?
Clearly, then, mental illnesses are a substantial blot on worldwide wellbeing. The next question is: what is being done about them at the moment? To shed light on this, this section compares the resources put towards mental vs physical health disorders, current mental health spending, and the treatment gap for mental illness.
4.1 Mental health receives disportionately fewer resources than physical health
In terms of national spending, in every country the proportion of the health budget spent on mental healthcare and research is disproportionate to the burden of mental disorders (see figure 4) (Patel et al., 2018). To be clear, this by itself does not show more should be spent on mental health, if the aim is to have the biggest impact using scarce resources: if interventions in other areas were more cost-effective, then this allocation would be justified. However, as we go on to argue, it seems likely mental health has been unduly neglected due to reasons such as stigma.
Less than 2% of median government health expenditure is on mental health, ranging from US$80.24 per capita in HICs, to US$0.02 in LICs (WHO Mental Health Atlas 2017). Commonly, countries do not have any separate budget for treating neurological or substance-use disorders (WHO Neurological Disorders Atlas 2017; WHO Substance Use Atlas 2010), so this mental health budget is divided among all MNS disorders.
In addition to the neglect by governments, mental health is neglected in development assistance. International development assistance is also important as development assistance funds 20-40% of primary healthcare spending in LICs (WHO, 2019c). From 2006-2016, the share of international development assistance specifically directed to MNS disorders was 0.3% (Liese, Gribble and Wickremsinhe, 2019). Development assistance from 2006-2016 for mental health was US$0.85 per DALY lost to the problem compared with $144 for HIV/AIDS and $48 for tuberculosis and malaria in 2013 (see figure 5) (Charlson et al., 2017). Mental health is therefore neglected compared to many other aspects of global health.
Mental health is also neglected in research funding. Investments in mental health research are disproportionate to the burden of mental health conditions in every country (Patel et al., 2018). The majority of research funding in LMICs is directed towards communicable diseases (WHO, 2019e).
Figure 4: A small proportion of health expenditure is allocated to mental disorders relative to the DALY burden they cause

Note: Column chart showing the burden of DALYs caused by mental health disorders compared to government expenditure on mental disorders, shown by World Bank income group. Adapted from Ridley et al., 2020, and data from GBD, n.d.
Policy commitments have increased, with many mental health policies being developed in the 1990s, but are yet to be followed up with financial investments (WHO Mental Health Atlas, 2005; Lund, 2019). Seeing as mental health has only recently become a concern for HICs, and mental health remains neglected in all countries, it seems reasonable to worry that increases in funding could take many years in LMICs.
Child and adolescent mental health is thought to be especially neglected (Patel et al., 2018). Mental and substance use disorders are the largest cause of YLDs among children and adolescents (Patel et al., 2018); however, very few mental health workers are available to provide child and adolescent services (WHO Mental Health Atlas 2017). A potential explanation for this is the difference in presentation of problems in childhood compared to in adulthood (Crick Lund, pers. comm., 2020), possibly contributing to the poor diagnosis and lack of treatment among children and adolescents (WHO, 2020a).
Figure 5: A small proportion of development assistance for health is allocated to mental disorders relative to the DALY burden they cause

Note: Column chart showing development assistance allocated in US$ per DALY for each disorder/group of disorders from 2012-2014. Figure adapted from Charlson et al., 2017.
4.2 Neglect results in a large treatment gap
The treatment gap for mental health disorders and substance use has been claimed to be larger than for any other health sector, although it is unclear how this conclusion was reached and how other “sectors” are defined (Trautmann, Rehm and Wittchen, 2016). A study carried out in 21 countries found that, on average, 84% of people with depression did not even receive “minimally adequate treatment” – the figure was 73% in high-income countries and rises to 94% in low- and middle-income countries (Thornicroft et al., 2017). Even fewer will receive “gold standard” treatments. If unreported mental illnesses were also included, then the treatment gap would be even greater (Yaro et al., 2020).
5. Depression and anxiety in LMICs: Are there (more) effective interventions?
Not only are mental illnesses large in scale, not much is being done about them. What can be done? What can be done better?
To make these questions more manageable, this report restricts its focus to depression and anxiety in LMICs. We do this because our expectation is that, in the category of mental health, this is the combination of illnesses and locations that contains the most cost-effective ways to improve lives. Focusing on cost-effectiveness is necessary if we want to do the most good with limited resources. This expectation is a result of the combination of: the per-person badness of these conditions and their high prevalence (see section 2); the existence of effective treatments (discussed in this section); the lower cost of labour in poorer settings; the relative additional neglect of mental health disorders in poorer settings anyway (as noted in section 4). Hence, this is where we expect the “lowest-hanging fruit” is.
We emphasise this view is not strongly held: we have not looked carefully either at other mental health disorders, or in other settings. We hope future research will explore and evaluate these alternatives.
In this section, we consider whether effective interventions exist and can be delivered at scale. We then highlight how resources are currently being spent.
5.1 Effective interventions exist
To a large extent, mental health disorders are both preventable and treatable (WHO, 2004; WHO, 2019a). This subsection provides a brief overview of the types of interventions available for reducing the global mental health burden. These interventions can be divided into three categories:
- Treatments: interventions for those who already have a disorder.
- Prevention: interventions that reduce the chance someone will get a disorder later (WHO, 2002; WHO, 2018).
- Promotion: interventions that aim to generate good mental health, rather than just tackling mental ill health. As noted, there is a difference between being happy and not being depressed.
Table 1 provides a non-exhaustive list of common prevention and treatment strategies for tackling anxiety, depression, and suicide. Effective preventive interventions for children and adolescents also exist, including life-skills curricula, parenting interventions, and protection from neglect or violence (Patel et al., 2018). Several systematic reviews have shown psychosocial interventions to be effective in LMIC settings (Patel et al., 2018). Recommended best-practice interventions include life-skills training in schools, diagnosis, management, and psychological treatment for depression and anxiety (Patel et al., 2016a).8Best practice interventions for mental health disorders were identified in the Disease Control Priorities report on the basis of evidence for their effectiveness, contextual acceptability and scalability in LMICs, and cost-effectiveness, at least in HICs (Patel et al., 2016a). Strategies for promoting mental health are not separately labeled below and often share an overlap with those for treating and preventing mental illness. Some specific promotion options include child development programmes, empowerment of women, social support for vulnerable groups, housing policies, poverty reduction, and anti-discrimination laws, among other things (WHO, 2018).
Table 1: Non-comprehensive list of common prevention and treatment examples for depression, anxiety, and suicide
| Disorder | Examples of Prevention and Treatment |
| Depression |
Prevention Exercise programmes for the elderly, school-based social and emotional learning programmes or parent training programmes (WHO, 2004) |
|
Treatment Psychosocial interventions, including cognitive behavioural therapy (CBT)9CBT is an umbrella term for multiple evidence-based psychological therapies (Gaudiano, 2008). CBT is effective for treating a variety of mental and substance use disorders; however, both the effectiveness and the quality of evidence varies between disorders (Hofmann et al., 2012). Antidepressant medications, including selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) |
|
| Anxiety |
Prevention Reducing incidence of (or exposure to) traumatic events, critical incident stress debriefing (CISD) following a traumatic event, and school-based social and emotional learning programmes (WHO, 2004) |
|
Treatment Psychological interventions, including CBT and psychoeducation Pharmacological interventions, including SSRIs and serotonin-norepinephrine reuptake inhibitors (SNRIs) |
|
| Suicide |
Prevention Hotlines and crisis centres, school-based programmes, training of practitioners to recognise and treat depression, and restriction of access to common methods of suicide, including pesticides, firearms and medications (WHO, 2004) |
|
Treatment Psychosocial interventions, including psychoeducation Prevention of depression, and alcohol and drug-use disorders Management of concurrent conditions |
Note: Information from WHO, 2008b; WHO, 2020b; WHO, 2008a; NICE, 2019; Kermode et al., 2011; Patel et al., 2016a; and Thakur et al., 2016.
If effective interventions like these were to be scaled up, the population-level burden of mental health disorders could be greatly reduced. It is worth noting that, if the current treatments were given to everyone who could use them, mental illnesses would not disappear entirely; Cuijpers et al. (2014a) show that, after psychotherapy treatment, 38% of of patients still had major depressive disorder, and Cuijpers et al. (2014b) show that antidepressant medications have an effect size similar to psychotherapy. Figure 6 illustrates the effectiveness of treatments for adult psychiatric disorders (not just depression and anxiety).
Figure 6: Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders

Note: Reproduced from Huhn et al. (2014). SMD = standard mean difference.
Effective, evidence-based treatments for mental illnesses are relatively recent, at least in comparison to those for physical health. Antidepressants entered clinical use in the 1950s (López-Muñoz and Alamo, 2009) and cognitive-behavioural therapy (CBT) was developed in the 1960s (Ruggiero et al. 2018). Given this, we might hope further research will yield more effective treatments, an issue we return to in section 7.1.
In addition to focusing directly on preventing, promoting, or treating mental illnesses, it is also possible to attack these indirectly via their social determinants. Aspects of genetics and biology are risk factors for mental health disorders (Patel et al., 2016a), and for many of these disorders, social, economic, and physical environments also have a large influence on a person’s vulnerability (WHO, 2014; WHO and Calouste Gulbenkian Foundation, 2014). For example, determinants of depression include conflict and civil unrest, environmental changes, income inequality, gender inequality, education, and poverty (Blas, Sivasankara Kurup and WHO, 2010). Addressing these social determinants requires action from outside of the health sector, for example the social, education, employment, housing, and justice sectors; however, these are not yet sufficiently involved in the prevention of mental illness and promotion of mental health (Patel et al., 2018; WHO, 2007; Collins et al., 2013; Deb and Gupta, 2017). Prevention and promotion may be especially promising given the limited effect sizes of treatments.
Addressing social determinants of mental health can involve community empowerment, people-centred health services, and patient and community knowledge and ownership (Burgess et al., 2019). Goals to work towards include reducing gender-based violence, child maltreatment, racial discrimination, and income inequality, as well as improving housing, social support and networks in older adults, neighbourhood safety, response to environmental events, and education (Lund et al., 2018). Social and emotional learning programmes have also been shown to have long-term and widespread benefits, and could be delivered by teachers and school counsellors (Levin and Chisholm, 2016; Reynolds et al., 2007; Wasserman et al., 2015). It is also important that we have suitable indicators to be able to measure progress towards these goals (Lund et al., 2018).
5.3 Prioritising child and adolescent mental health
Child and youth mental health is currently thought to be more neglected than disorders in adulthood and needs to be prioritised (Patel et al., 2018). Investing in interventions for this age group may be more impactful, as most mental disorders originate in childhood, and early intervention is likely to prevent problems in later life (Patel et al., 2018; Patel and Saxena, 2014).10 It is noteworthy that the focus on depression and anxiety may be less relevant when considering child and adolescent mental health. Other disorders of importance among young people include neurodevelopmental disorders, conduct disorder, ADHD, oppositional defiant disorder, and substance use disorders. Early recognition of a mental health disorder may be more effective, can help to reduce stigma (Patel et al., 2018), and can prevent the suffering experienced prior to diagnosis and treatment.
5.4 Strategies exist for scaling-up delivery of interventions
In addition to the existence of effective interventions, there is also a need for effective methods of delivery. This is especially challenging given the shortage of resources and mental health professionals. This section outlines two promising strategies that, at least in theory, can allow scale-up of treatment without intensive use of professionals’ time: task-sharing and use of digital platforms. While affecting healthcare systems globally, the COVID-19 pandemic has hastened the transition towards these two strategies (Vigo et al., 2020).
Innovation also has an important role to play in scaling up treatments. There is much to gain from the sharing of ideas and innovations between all settings, including mutual learning between high resource settings and low resource settings (Collins and Saxena, 2016). In addition to such knowledge sharing, innovations must be adapted to suit local needs (Collins and Saxena, 2016).
5.4.1 Task-sharing
One strategy that has been shown in trials to be effective is task-sharing (Nadkarni et al., 2016; Patel et al., 2017). Task-sharing refers to the training and supervision of lay health workers by professionals, for example providing them with the knowledge and skills to deliver psychosocial interventions (Patel, 2009; Saraceno et al., 2007; WHO, 2007). Task-sharing has been shown to improve outcomes for people with mental disorders (Kakuma et al., 2011), and can be used in LMICs to overcome human resource shortages and increase coverage of care (Patel, 2009). However, questions remain regarding how to scale up most efficiently using task-sharing, such as the number and content of sessions to be delivered, and the extent of training required for the lay health workers (Lund et al., 2019). Some experts have also called for increased use and support of non-formal resources, such as families and neighbours (Saraceno et al., 2007).
A stepped-care approach would also be beneficial for scaling-up of psychosocial therapies whilst reducing professional involvement (Patel et al., 2018). This involves matching the intensity of care to the severity of the disorder. For example, a first step might consist of self-delivered interventions for mild to moderate conditions, a second step might include psychosocial therapy delivered in routine care by lay health workers, and a third step might include consultation with a specialist, medications, or more complex psychotherapies (Patel et al., 2018).
5.4.2 Digital platforms
A second option for delivery is through digital platforms, which have been demonstrated in trials to be effective (Andrews et al., 2019; Firth et al., 2017). A recent meta-analysis of digital psychological interventions in mental healthcare suggests that these are a promising option for LMICs, especially in areas where mental healthcare is minimal or absent (Fu et al., 2020). These interventions have mainly been studied among individuals with depression or substance-use disorders, and were found to be more effective than usual care (Fu et al., 2020). However there is substantial heterogeneity in the effectiveness of digital interventions and no conclusions could be drawn about long-term impacts due to short follow-up periods (Fu et al., 2020).
The Lancet Commission encourages increasing use of digital technologies (Patel et al., 2018). eHealth can be used for multiple aspects of care delivery, including, for example, training health workers, improving diagnosis, increasing adherence to treatment, and delivering self-help programmes (Naslund et al., 2017). Although digital technologies can provide great potential benefits, attention should be paid regarding risks to efficacy, privacy and confidentiality (Patel et al., 2018).
Ethical concerns, especially data privacy and individual rights, are barriers to the use of digital technology (Doraiswamy et al., 2019). Actions must be taken to address these problems (Doraiswamy et al., 2019), however these barriers can likely be mitigated by altering delivery and monitoring. Low adherence to digital interventions is a further issue to be addressed (Christensen, Griffiths and Farrer, 2009; Melville, Casey and Kavanagh, 2009).
5.5 Current cost-effectiveness estimates for interventions in LMICs are limited
Disease Control Priorities (DCP) laments the “dearth of information on cost-effective interventions for mental health in LMICs” (Horton, 2016). Very few studies of cost-effectiveness have been carried out in low-income and lower-middle-income countries (see table 2) (Horton, 2016; Patel et al., 2016a), and often international estimates are used, rather than estimates of the cost for a specific location (Levin and Chisholm, 2016). This is a limitation as the costs of an intervention can vary greatly between locations due to, for instance, labour costs.
The third edition of the Disease Control Priorities contained the most recent large-scale review (covering literature up to 2013) of cost-effective interventions for MNS disorders (Levin and Chisholm, 2016).
In the papers cited above, there is a wide range in cost-effectiveness estimates, and the majority of interventions are significantly less cost-effective than those in table 2. Disease Control Priorities therefore cautions that we should choose and carefully evaluate appropriate interventions before scaling up (Levin and Chisholm, 2016). One source of cost-effectiveness estimates is the Draft WHO Policy Options Menu, which groups interventions into four cost categories per DALY averted: <$100, $100-500, $500-1000, and $1000-5000 (WHO, 2019f).
Table 2: The most cost-effective interventions for mental health disorders identified during research for this report
| Intervention | Cost-effectiveness in US$ per DALY averted | References |
| Preventing suicide through regulation banning hazardous pesticides. | <US$100 | WHO, 2019f |
| Provision of psychosocial support and antidepressants on a maintenance basis for moderate to severe cases of depression. | <US$100 | WHO, 2019f |
| Psychological treatment on a maintenance basis for recurrent moderate to severe depression. | <US$100 | WHO, 2019f |
| Episodic treatment with antidepressant drugs in primary healthcare in South and East Asia and the Pacific. | US$786-US$899* | Levin and Chisholm, 2016 |
Note: The prices shown are largely cost estimates for population-level coverage, rather than for small-scale interventions. *price dependent on location.
It is possible that provision of treatment among specific subgroups could be more cost-effective. Mental health interventions can also lead to physical health improvements which are not easily accounted for in cost-effectiveness analyses. As an example, screening for depression and provision of fluoxetine among people living with HIV in sub-Saharan Africa was found to improve HIV treatment outcomes and is estimated to cost only US$15 per QALY (Zhong et al., 2020).
These cost-effectiveness estimates should persuade governments that mental health disorders are a promising area. To draw the comparison between HIV and mental health disorders, costs of prevention and treatment for HIV varied between US$46 and US$303 per DALY averted when making various assumptions about effectiveness and compliance (Garnett et al., 2017). It seems that well-chosen mental health disorder interventions can be similarly cost-effective; however, in development assistance, 169-times more was spent on HIV/AIDS per DALY than on mental health (Charlson et al., 2017).
The only cost-effectiveness estimate we are aware of for a philanthropic intervention in terms of $ per DALY averted is Founders Pledge’s evaluation of StrongMinds. StrongMinds runs an intervention in which local professionals are trained to deliver Interpersonal Group Psychotherapy to women with depression in Uganda, which Founders Pledge estimates costs US$377 per DALY (Founders Pledge, 2019; StrongMinds, n.d.). If DALYs are the outcome metric, then this is currently less cost-effective than GiveWell-recommended charities such as the Against Malaria Foundation (AMF) which provides antimalarial bednets for an estimated US$78 per DALY (Giving What We Can, 2016).11It should be noted that GiveWell no longer evaluates the cost-effectiveness of charities in terms of $ per DALY (GiveWell, 2020).
An important consideration is that the cost-effectiveness estimates are in terms of DALYs, rather than in terms of subjective wellbeing (SWB). As mentioned previously, DALYs likely systematically underestimate the true SWB burden of mental disorders (relative to physical health disorders). There is already reason to believe that cost-effectiveness of mental health interventions may be promising when measured in terms of SWB (Plant, 2018; 2019; Founders Pledge, 2020). The Happier Lives Institute is currently working on assessing the cost-effectiveness, as measured in SWB, of several global health and development interventions.
Further analysis could identify more highly cost-effective interventions. For example, there is a need for cost-effectiveness estimates for training gatekeepers to identify mental illness, social and emotional learning programmes, laws and regulations to reduce alcohol-use disorders, community-based parenting programmes, and self-care such as via e-health (Levin and Chisholm, 2016).12Some researchers argue that cost-effective interventions already exist, and that, instead, research is needed on how to implement and scale-up those treatments to deliver mental healthcare (see more in Section 7.1) (Vikram Patel, pers. comm., 2020).
5.6 Existing resources are largely spent on ineffective mental hospitals
Despite current investments being exceptionally small, these are both ineffectively spent and in some cases underutilised. Of public expenditure on mental health in LMICs, 80% is currently spent on mental hospitals (see figure 7) (WHO Mental Health Atlas 2017). Spending on community-oriented, person-centred care, and on integration in routine health and social-care platforms, is therefore negligible (Patel et al., 2018). Psychiatric hospitals are often located near cities (Saraceno et al., 2007), separated from the community and built decades ago (Patel et al., 2018). The conditions within psychiatric hospitals in LMICs are typically poor. Lack of shelter and food, overcrowding, unsanitary conditions, and physical abuse have been reported, as well as poor quality of care (Drew et al., 2011; Patel et al., 2018).
Political support, increased investment, and reallocation of physical health budgets are all needed in order to transition away from providing care in mental hospitals to providing community-based care (Saraceno et al., 2007; Saxena et al., 2007; Patel et al., 2018), creating a barrier to change. Less significantly, mental health professionals may have incentives to maintain the status quo, such as fear of being relocated to rural areas if services are shifted to community-based care, and hospital directors may resist losing their current power (Saraceno et al., 2007). There is a risk that trade-union protests would make this transition more difficult (Saraceno et al., 2007; WHO, 2007).
Instead of psychiatric hospitals, more cost-effective community-based services can be provided, which would be expected to increase access to care (WHO, 2013b; Wiley-Exley, 2007; Patel et al., 2018; Thornicroft, Deb and Henderson, 2016).13Deinstitutionalisation has been taking place in HICs for more than 50 years (Thornicroft, Deb and Henderson, 2016). Evidence from HICs suggests that community-based care is more cost-effective in terms of quality of life and life satisfaction than hospital-based care (Thornicroft, Deb and Henderson, 2016). However, downsizing of hospitals would need to be accompanied by increased investment in community-based services, rather than with the aim of reducing total costs (Thornicroft, Deb and Henderson, 2016). Community-based services can include supported housing and community-based mental health workers (Killaspy, 2007). A shift away from psychiatric hospitals and towards community-based care has been taking place over several decades in HICs and positive outcomes have been demonstrated (Thornicroft, Deb and Henderson, 2016), including for individuals who had been living in such hospitals (Killaspy, 2007). However, Dias and Fontes (2020) reviewed the implementation of a deinstitutionalisation programme in Brazil and found that, while it had several benefits, it did lead to an increase in homicides; these were particularly associated with violence by schizophrenic males under-40, who would previously have been hospitalised. Therefore, a move away from psychiatric hospitals should be done with care, making sure adequate support is provided to vulnerable groups.
The Lancet Commission for mental health recommends a balance between community-based and hospital-based components (Thornicroft and Tansella, 2013), although the details differ by income group (Patel et al., 2018) and depend on local circumstances (Thornicroft and Tansella, 2013).
Relatedly, mental health services are not accessible within primary healthcare (WHO, 2007; Patel et al., 2018; Saraceno et al., 2007; Esponda et al., 2020). Integrated care for mental health has been under-prioritised and under-funded (Esponda et al., 2020). Primary healthcare workers are already overburdened, and do not always have time to provide care to people with mental disorders (Saraceno et al., 2007). Most patients prefer psychosocial interventions when given a choice (Patel et al., 2018); however, due to lack of physician time, patients who prefer counselling may be given medication instead (Andrade et al., 2014). This is important in light of results showing greater efficacy when patients receive their preferred treatment option (Kocsis et al., 2009). Investments are needed to strengthen health systems to manage the increased burden of treating mental health disorders (WHO, 2019e; Esponda et al., 2020), especially in order to provide the chronic care needed for some mental disorders, which differs from the episodic and acute care these systems have largely been developed for (Petersen et al., 2019). Integration of mental health services within primary healthcare would likely bring great benefits in both HICs and LMICs (Patel and Chatterji, 2015).
Figure 7: A high proportion of total government expenditure on mental health is spent on psychiatric hospitals

Note: Column chart showing government expenditure (including national and subnational spending) on mental health and on psychiatric hospitals per capita (US$), by World Bank income group. Figure adapted from WHO Mental Health Atlas 2017.
Mental health is also not well integrated with other health programmes (Patel et al., 2018), such as maternal, sexual, reproductive and child health, HIV/AIDS, and other NCD programmes (WHO, 2007; WHO, 2013b). In addition mental health disorders need to be integrated into the wider global health agenda including universal health coverage (Patel et al., 2018).
6. Why aren’t people getting (the most) effective interventions? The role of stigma
As we can see, steps could be taken to tackle this problem, and to tackle it more effectively. Why hasn’t this happened so far? This section takes a backwards-facing, general perspective on why the problem hasn’t been solved so far.14 Or, more precisely, has been solved in the matter and to the extent that it has been solved. The next section looks forward and considers some actions for donors and those seeking high-impact careers.
As we have seen, the treatment gap for mental illnesses is enormous in both richer and poorer countries (4.2). If the treatment gap didn’t exist in rich countries, the obvious explanation would be that poorer countries had not prioritised this due to cost. While the total amount of resources societies have clearly plays a role, it seems the relative lack of funding, attention, and research that mental illnesses have received is substantially due to stigma and misunderstanding, an issue that is relatively worse in poorer countries.
Stigma affects multiple different actors and is a significant barrier to making progress. Stigma is prevalent among health professionals (Knaak, Mantler and Szeto, 2017; Knaak, Ungar and Patten, 2015), communities, and among people living with mental health disorders themselves (Andrade et al., 2014).
There are multiple mechanisms through which stigma and misunderstandings can contribute to the financial neglect of mental health disorders. For example, lack of awareness of the value of mental health for social and economic development and a lack of general public interest in mental health have both been noted (WHO, 2007; Patel et al., 2018). There is also a misconception that mental disorders can’t be treated (National Alliance on Mental Illness, 2015) and decision-makers are rarely aware that cost-effective interventions (often defined as costing less than three times the GDP per capita per DALY averted) exist (WHO, 2007).
Stigma among health professionals is also believed to act as a barrier to access and quality of care, and drives students away from careers in psychiatry (Kakuma et al., 2011). Globally there are nine mental health workers per 100,000 population, varying from 1.6 in LICs, to 71.7 in HICs (see figure 8) (WHO Mental Health Atlas 2017), making up only 1% of the global health workforce (WHO, 2015b). Mental health training is not commonly given to general healthcare workers, and training for medical students is insufficient (Saraceno et al., 2007): less than 2% of physicians and nurses globally received training to recognise and treat mental disorders in the previous year, and data on the proportion trained is lacking from many countries (WHO Mental Health Atlas 2017).
Several factors likely deter people from working in mental health, especially in rural areas. Mental health professionals often have poor working conditions, low status, and wages are often higher in private practice and in other countries (Saraceno et al., 2007). It is common for mental health professionals from LMICs to migrate from rural to urban areas, or emigrate to HICs (Jenkins et al., 2010; Kakuma et al., 2011).
The perception that one’s own mental health problem does not need treating is widespread, especially among people with moderate and mild disorders, and many people desire to deal with the problem alone, likely due to the stigmatising views held by a person with a mental disorder about themself (Andrade et al., 2014).
As a result, stigma prevents individuals from seeking treatment and therefore demand for services is low (Saxena et al., 2007; Patel et al., 2018). In a survey across 21 countries, only one in three people with depression in LMICs recognised the need for treatment, compared to two out of three in HICs (Thornicroft et al., 2017). Lack of demand for services is thought to contribute to the lack of funding for mental health services in LMICs (Mascayano, Armijo and Yang, 2015). Not only is initial demand for services low, but follow-up and adherence to care are also poor (Patel et al., 2018). Due to stigma worsening some people’s mental health problems and preventing them seeking treatment, stigma and discrimination may trap people in a cycle of illness (Mental Health Foundation, 2015).
Figure 8: The global mental health workforce is small and particularly limited in LMICs

Note: Column chart showing mental health workforce per 100,000 population, by World Bank income group. Adapted from WHO Mental Health Atlas 2017.
An upcoming Lancet Commission aims to address stigma and discrimination in mental health, including its adverse impacts, the cost-effectiveness of interventions, as well as recommended policies, initiatives and next steps (Thornicroft and Sunkel, 2020).
7. What can be done?
This section provides some options for donors, and for individuals aiming to have high-impact careers, who want to put their resources towards improving global mental health.
Two caveats. First, we have not attempted to prioritise among these actions: not only is this outside the scope of this report but is very challenging to do, particularly regarding individuals wondering how to do the most good with their professional lives as this will heavily depend on their personal fit for various roles. For readers curious about having a high-impact career, we recommend 80,000 Hours, which provides some excellent generic advice on this topic (80,000 Hours). Second, in what follows, we mention a number of organisations individuals could potentially work for and that donors might fund. However, this selection is neither exhaustive or systematic, and is largely drawn from those we are familiar with.
7.1 Research
Many unanswered questions remain in the field of mental health. Donors could fund research into these or individuals, if correctly positioned for an academic career, could undertake them themselves.
Indeed, the breadth of open research questions is so diverse that we believe it would be valuable to undertake a project prioritizing mental health research topics and strategies. It is likely that avenues of research differ in their potential impact by orders of magnitude, and some prominent researchers have expressed concern that some investments in mental health research on topics such as genetics and biomarkers15Biomarkers are substances which can be detected in blood or urine indicating increased risk of a disorder. have, at least to date, failed to “move the needle” in real-world impact (Rogers, 2017; Vikram Patel, pers. comm., 2020). However, to our knowledge, no attempts have been made to comprehensively quantify the relative cost-effectiveness of research programs that could improve mental health, looking from the farthest “upstream” basic science to the most “downstream” research investigating service delivery. Although groups of researchers, advocates, and other stakeholders have proposed lists of major tasks in mental health research (see, e.g., Box 2), these lists do not compare the items, and they omit some promising options. Even a “back-of-the-envelope” analysis of the best (and worst!) research opportunities would be of use, and though it may not influence established investigators to change course, it could be a substantial benefit to those planning research careers and those selecting funding opportunities as well as a guide to the field moving forward.
Such a project would need to consider the mental health research field broadly, looking across at least two dimensions: first, interventions used prior to someone having a mental illness, i.e., prevention (and promotion), versus interventions used once an illness is present, i.e., treatments; and second, developing novel interventions, versus enhancing the impact of existing interventions, versus expanding access to existing interventions. (Note that this taxonomy does not exclude basic research on, for example, the causes and dynamics of mental illness, which is deeply valuable for informing applications.) Box 2 lists several examples of research in each category, but note that the review is far from comprehensive and does not constitute a recommendation of any particular area.
The process of prioritizing research programs could use a variety of approaches for modeling their costs and benefits, but should at minimum take into account:
- The number of people who would benefit from a particular advance and the degree to which they would benefit;
- The tractability of the problem from a scientific/technical standpoint as well as a social/political/structural standpoint, i.e. accounting for what might be publicly acceptable in the future, including the costs of the research itself and the efforts needed to bring findings to bear;
- And the pace and effectiveness of current progress on the issue, including the primary bottlenecks to progress.
As an example of how these questions might guide research priorities, one could compare :
- the application of genetic research to developing novel interventions for preventive purposes, to
- the application of implementation science to expanding access to existing interventions for treatment purposes
(note that both of these fields could have applications in other categories in the taxonomy).
Given that most mental illnesses are around 50% heritable, even higher for some disorders, intervening on genes might be the single most powerful way to prevent mental illness.16If, say, 50% of variance in a characteristic, like poor mental health, is due to genes (see e.g McInnis and Zöllner, 2008) the “left-over” 50% is typically called “environmental” variance and is often implicitly assumed to be malleable. However, it would be more accurate to call the left-over 50% “non-genetic,” and there is no guarantee that those factors are malleable. Some portion of the left-over variance may simply be stochastic–like whether a growing neuron “zigs” or “zags” in a developing fetus. Other environmental events that contribute to variance may also be unpredictable and not amenable to intervention (as a silly example, whether someone trips and hits their head as a child). All of this shrinks the amount of variance in mental illness that one could affect by intervening during an individual’s life, strengthening the possibility that genetic intervention would be substantially more powerful than environmental interventions. (On the other hand, there may also be cases in which what appears to be “genetic” variance could be impacted by changing the environment. Imagine, for example, a fictional gene that makes drinking alcohol irresistible and thus increases the risk for alcohol use disorder. In an environment where alcohol is readily available to everyone, this risk factor would “show up” in the genetic portion of the risk for alcoholism, but it would be possible to intervene by ensuring that individuals with the gene do not have access to alcohol.) See Jasanoff (2018) for a popular-press review of the complex pathways through which genes and other factors can interact to influence the brain and behavior. In terms of tractability, progress has historically been slow in identifying genetic variants that increase risk for mental illness, but has recently accelerated through advances in methods and data availability (Merikangas & Merikangas, 2019; Smoller, 2017). However, many additional research steps are needed to put these basic findings to use. Further, the social and political hurdles to directly editing genes may be insurmountable in the short term, although fortunately, there are numerous other potential applications for genetic research (e.g., improving taxonomies and definitions, identifying targets for new treatments, and personalizing treatment; Smoller, 2017).
In contrast, implementation science is a multidisciplinary area of research that investigates how to facilitate sustained adoption of evidence-based interventions, programs, and policies (Bauer et al., 2015; UW Implementation Science Resource Hub, n.d.). Since many promising advances fail to scale up (or to reach the public at all), implementation science may prove essential to ensuring that the fruits of any type of mental health research are successfully applied. On the other hand, it would be reasonable to question the value of additional investment in some forms of implementation science. For example, research aimed at disseminating existing evidence-based psychotherapies to professionals currently providing treatment in HICs may not be as cost-effective as other ways to promote mental health: evidence-based psychotherapies may only be slightly more effective than what therapists do in routine practice (although the size of the difference remains controversial; McAleavey et al., 2019; Nordmo et al., 2020), and training therapists who are already practicing in the community to adopt evidence-based practices has proven costly and challenging (Beidas & Kendall, 2010; Beidas et al., 2019).
A project aimed at prioritizing mental health research would elaborate on these considerations and quantify the expected costs and benefits of various research programs accordingly. These are only two examples of research areas; Box 2 lists more possibilities for using research to promote mental health, covering all six groups in the taxonomy.
A comprehensive prioritization of mental health research opportunities would require domain expertise and consultation with scientists in multiple fields. But given the importance of mental health and the sheer number of options for those wishing to promote it, even roughly sorting fields and questions into a few strata based on orders of magnitude would provide valuable guidance. Until such a task is undertaken, those wishing to fund or pursue a career in mental health research may want to investigate some of the questions above themselves when selecting among choices (and ideally, could share what they learn with others).
|
Box 2: Promising research directions Published lists of research priorities Individuals interested in promoting mental health through research may find it useful to review published lists of major open questions and goals that have been identified by those working in the field. The Grand Challenges in Global Mental Health identified the top challenges that can be addressed through research (Collins et al., 2011), and the Lancet Commission later built on these research priorities (Patel et al., 2018). There are six goals for mental health research outlined by the Grand Challenges report:
Other calls for research in the literature are often in line with these six goals. Mental health experts representing a wide range of sectors recently convened and identified a further list of research priorities, including demographic, economic, environmental events, neighbourhood, and sociocultural research (Rose-Clarke et al., 2020). These priorities overlap with those mentioned above, although suggest additional avenues for further research such as the relationship between mental health and social protection measures, cash transfers, and neighbourhood and community resilience (Rose-Clarke et al., 2020). The COVID-19 pandemic has brought to light the mental health consequences of a public health emergency and research is necessary in order to learn from this crisis and better prepare for future events (Vigo et al., 2020; Maulik, Thornicroft and Saxena, 2020). A taxonomy of research areas As noted in the text, one way of dividing up mental health research questions would be along two dimensions (some of which correspond to the priorities listed above):
Research into prevention and promotion may be especially impactful, in light of the small effect sizes of existing treatments, the difficulty of altering some of the causes of mental illness once they are already present, and the additional suffering that can be averted by ensuring that a mental illness never develops. Research elucidating the causes of mental illness could contribute to prioritizing possible prevention methods. Although a great deal of progress has already been made in this regard, identification of the specific genes involved in risk for mental illness and their mechanisms of action has only recently accelerated; with regard to environmental causes, further work could clarify whether some potential risk factors play a truly causal role, the relative magnitude of various causes, and the mechanisms by which they lead to mental illness. This research could not only contribute to identifying targets for developing novel preventive interventions, but also could help select among existing preventive interventions. Existing prevention methods focus primarily on social determinants of mental health (Lund, 2019; Burgess et al., 2019). The range of possible prevention strategies for mental health disorders is vast, for example spanning from lead abatement to social and emotional learning programmes (Reuben et al., 2019; Levin and Chisholm, 2016). Estimating the costs and effectiveness of prevention strategies would likely be valuable. More research is needed to understand the long-term mental health benefits that can be gained from such interventions (Burgess et al., 2019), and inclusion of more risk factors in the GBD would also help to better prioritise among risk factors and may increase the attention paid to prevention (Harvey Whiteford, pers. comm., 2020). Research aimed at expanding access to and enhancing some of these preventive interventions falls in the domains of implementation science and social sciences (e.g., economics, policy, and law) and might investigate questions regarding, for example, the regions in which raising taxes on alcohol is most feasible and how to increase buy-in from the public or policymakers. With regard to treatment, identifying more potent options is a key area for future research (Wainberg et al., 2017). Although effective treatments exist which, if scaled up, could greatly reduce the population-level burden of mental health disorders, they are far from perfectly effective; even if every individual living with a mental health disorder were to receive the current best evidence-based treatment, many individuals would still experience some symptoms. Taking depression as an example, antidepressant medications are significantly more effective than placebo pills, but the effects of such medications have been overestimated in the literature due to publication bias (Turner et al., 2008; Cuijpers et al., 2014). There is a similar picture emerging for psychotherapy: CBT is significantly more effective than a placebo pill, but with an effect size of only around d = 0.25 (Cuijpers et al., 2014), comparable to that of antidepressants. Recent developments suggest that exploring entirely new treatment paradigms may be one way to identify substantially more powerful treatments. For example, psychedelic-assisted psychotherapy involves one or more long (e.g., 6+ hour) treatment sessions with a psychotherapist while medicated with a drug such as MDMA or psilocybin, which seem to potentiate the effects of psychotherapy. Such treatments have shown impressive results in small and open-label trials for a variety of disorders, including depression, anxiety, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and substance use disorder, and are currently undergoing large-scale trials (Griffiths et al., 2016; Mithoefer et al., 2019; Moreno et al., 2006; Johnson, Garcia-Romeu and Griffiths, 2016; Bogenschutz et al., 2015; Plant 2017). Founders Pledge considers the two best funding opportunities in psychedelic-assisted psychotherapy to be the Multidisciplinary Association for Psychedelic Studies (MAPS) and The Usona Institute (Founders Pledge, 2020). (It should be noted that many novel treatments perform well in initial trials but show smaller effects in later studies, and still smaller effects when delivered in practice, for a variety of reasons.) Examples of other treatment paradigms that go beyond traditional talk therapy or long-term medication use include non-invasive brain stimulation methods (Brunoni et al., 2017), stellate ganglion block injections for PTSD (Summers & Nevin, 2017), or even immunoregulatory nasal sprays (Amoroso et al., 2019). Some of these have demonstrated efficacy over decades of research; others are only beginning to be studied. Nevertheless, it is clear that the space of possible ways to affect mental illness has only begun to be explored, and basic research on mental illness that could inspire new treatments as well as applied research testing those treatments have the potential for high impact. Other developments suggest the utility of enhancing the impact of existing treatments, including through some relatively simple and low-cost means. Precision medicine, which is intended to match the right treatment to the patient and thus achieve larger effects through existing means, has generated a great deal of enthusiasm. Although some have been disappointed with its results so far in the mental health field, there has been progress in improving outcomes by developing algorithms for matching patients to different types of psychotherapy (Bickman, 2020; DeRubeis, 2019). Other simple changes that seem to enhance effects of psychotherapy include changing the dosage and frequency (e.g., Hansen et al., 2018) and adding simple exercises to help patients remember the content of their therapy sessions (Harvey et al., 2014). |
7.2 Intervention delivery
Intervention delivery refers to providing individuals with interventions that prevent or treat mental illness, or promote good mental health. This direct work could be carried out by funding, founding, or joining effective non-profit or for-profit organisations (80,000 Hours, 2014).
Non-profit organisations can serve a very valuable role, particularly in low-income settings where governance is weak, such as conflict-affected regions (where the prevalence of mental disorders is exceptionally high) or in locations where the local government has no reach, such as rural or remote areas (Vikram Patel, pers. comm., 2020). NGOs can also be innovative in ways that governments are less likely to be, for example by finding new ways to improve effectiveness or lower costs and may be able to encourage governments to scale-up services, such as Sangath’s work with the state government in India (Vikram Patel, pers. comm., 2020; Sangath, n.d.).
The most complete list of organisations working in global mental health we are aware of is provided by the Mental Health Innovation Network. It identifies 360 ‘organisations’ worldwide, although it is worth noting many of these are or were research projects which never got turned into an organisation implementing the intervention. The WHO’s Mental Health Atlas provides information on mental health resources worldwide but does not state which non-governmental organisations are working in this area.
As noted above (section 5.5), not much work has been done to assess the cost-effectiveness of non-profits and one mental health organisation, StrongMinds, has been estimated to be less cost-effective than certain charities evaluated by GiveWell. If, however, cost-effectiveness were to be measured in terms of subjective wellbeing, StrongMinds may be of higher impact than the GiveWell top recommendations (Plant, 2018).
At the Happier Lives Institute, we have been investigating possible donation opportunities as part of our Mental Health Programme Evaluation Project (Happier Lives Institute, 2020). For this project, we screened the 76 programmes that were (at the time) listed on the Mental Health Innovation Network database as focused on depression or anxiety. We narrowed down to the 12 that seemed most promising and are collecting information from implementing-organisations to, if possible, determine their cost-effectiveness. In the near future, we should be able to report cost-effectiveness estimates in terms of SWB andhow they compare to currently highly-regarded donation opportunities, e.g. those recommended by GiveWell.
Given the size of the treatment gap and the scope for innovation, we would be excited to see new mental health charities being started and experimenting with different delivery methods. Charity Entrepreneurship, a non-profit incubator (and research collaborator of HLI), provides guidance to those wishing to start new charities; they have produced a recommended list of speculative new mental health and happiness projects (Charity Entrepreneurship, 2020). Further, Canopie, an organisation providing mental health programmes to mothers, was founded about Charity Entrepreneurship’s incubation programme in 2020. At present, efforts to start such organisations seem constrained by funding: there does not (yet) seem to be a large donor base for effective mental health charities. The result is an unfortunate ‘chicken-and-egg’ problem: unless donors believe there are effective mental health charities, they will not fund them; without the prospect of funding, it is difficult for new, aspirationally impactful organisations to start.
For-profit work in technology entrepreneurship seems very promising. One well-known example of a for-profit digital intervention for improving wellbeing is Headspace, a meditation app, which has been evaluated in several trials (Headspace, 2020). Other technology products known to us include Happify (happiness-training exercises), MindEase (anxiety-relief), UpLift (computerised CBT for depression), and Sanvello (a support platform for mental health).17 Disclosure statement: Happify’s Chief Scientist is Sam Bernecker; MindEase’s CEO is Peter Brietbart. Sam and Peter are both trustees of the Happier Lives Institute. We understand such technology is still in its infancy. The challenge for it is the extent to which it can both effectively improve mental health and be commercially viable; we do not consider ourselves well-placed to judge either issue. However, if impactful, profitable products did exist, that would make an enormous dent in the burden of global mental illness. Such interventions are likely more relevant to HIC contexts, given the greater availability of computers and smartphones.
7.3 Policy and advocacy work
Between research that enhances our understanding of mental health, and efforts to deliver the interventions that directly improve it, there is also scope for valuable policy and advocacy work. This third option includes targeting decision-makers in private or public institutions, such as governments, and encourages them to take action, as well as efforts to raise awareness about mental health among members of the public. This might involve trying to make change from the outside, such as through grassroots campaigns, lobbying, or journalism, or working within a given organisation to alter its activities, for instance as a civil servant. Note those engaged in research and intervention delivery can undertake policy and advocacy alongside their other activities. As one example of advocacy, stigma reduction is discussed in Box 3, and a number of organisations working on policy and advocacy are mentioned in Box 4.
Inefficiency of current advocacy efforts has been identified as a barrier to progress in global mental health (WHO, 2007; Patel et al., 2018; Saraceno et al., 2007). Currently, different groups, such as clinicians, civil society, or economists, take different approaches to advocacy, passing contradictory messages to decision-makers (WHO, 2007; Patel et al., 2018). Improvements in advocacy could involve greater coordination of these messages, clearer communication to decision-makers (WHO, 2007; Saraceno et al., 2007), and better use of evidence of the efficacy of psychosocial interventions in LMICs to inform decision-makers (Barbui et al., 2020).
|
Box 3: Reducing stigma and discrimination The Time to Change campaign, which ran between 2007 and 2021, provides an example of advocacy to reduce stigma, aiming to change the way that people think about mental health (Time to Change). Work carried out by this organisation included working with employers to change attitudes to mental health in the workplace, supporting schools to deliver assemblies and lessons on mental health, and supporting individuals with lived experience of mental health disorders to share their stories and advocate for their rights. Attitudes towards mental health disorders were found to have improved among the individuals reached by these initiatives. Stigma-reduction interventions commonly involve providing factual information about mental disorders to the general public and to health professionals (Patel et al., 2018; WHO, 2001; Andrade et al., 2014; Clay et al., 2020). Enabling contact between the public and people with the stigmatised condition has the strongest evidence base of all interventions (Patel et al., 2018; INDIGO Network, n.d.). Digital technology can assist with anti-stigma campaigns and can be used to share lived experiences (Patel et al., 2018). Currently a wide variety of methods are in use globally for reducing stigma; however, more research is needed into the efficacy of these interventions, including longer follow-up periods and increased use of local expertise (Clay et al., 2020). Attempts to reduce stigma can be harmful, for example by increasing pessimism and even impeding recovery among affected individuals (Kvaale, Haslam and Gottdiener, 2013). It is important that people with lived experience of mental health disorders are empowered and included within advocacy efforts, as exemplified by the Mental Health Users Network in Zambia (Saraceno et al., 2007; MHUNZA, 2003). Importantly, there is no one-size-fits-all strategy, and the approaches or messages used to reduce stigma must be culturally appropriate to each setting (Patel et al., 2018; WHO, 2019e). The majority of studies of stigma have been carried out using Western-developed measures of stigma (Yang et al., 2014). The “What Matters Most” framework has therefore been developed to identify aspects of stigma that are culture-specific (Yang et al., 2014), and it has been so far utilised to better understand stigma in Chile and among Chinese immigrants in the US (Mascayano, Armijo and Yang, 2015; Yang et al., 2014). |
|
Box 4. Assorted policy and advocacy organisations
|
Concluding remarks
Mental health disorders are a large and neglected aspect of global health. They have a huge impact on wellbeing, are associated with significant stigma, and cause multiple challenges for the individual, their friends, and their family. Mental health is neglected worldwide due to the stigma surrounding these disorders and policymakers’ higher prioritisation of reducing infectious disease compared to improving wellbeing.
Despite the immense suffering caused by these disorders, there may be reason for optimism. Examples of low-cost interventions appropriate for LMIC contexts include delivery of psychotherapy through task sharing, digital technology, or integration of services within primary healthcare.
There are a multitude of potential avenues for reducing global suffering due to mental health disorders. As this report has highlighted, there are a range of options for donors and those aspiring to have impactful careers spanning research and directly providing interventions, as well as advocacy and policy.
Further reading
Overview
Overview: The Lancet Commission on global mental health and sustainable development; Return on Investment: Time to Invest in the Individual, 2020
Scale
DALY burden: Global Burden of Disease Results Tool
Underestimated DALY burden: Vigo, Thornicroft and Atun, 2016
SWB burden: Happiness Research Institute, 2020; Peasgood, Foster and Dolan, 2019
Economic burden: Bloom et al., 2011; Knapp and Wong, 2020
Physical health burden: WHO, n.d.-b; Stein et al., 2019
Neglectedness
Neglectedness: Saxena et al., 2007
Government funding & workforce: WHO Mental Health Atlas 2017; WHO Neurological Disorders Atlas 2017; WHO Substance Use Atlas 2010
Development assistance: Liese, Gribble and Wickremsinhe, 2019; Charlson et al., 2017
Barriers to progress
Barriers: Saraceno et al., 2007; WHO, 2007; Andrade et al., 2014
Interventions and solutions
Social determinants and prevention: WHO, 2014; Lund et al., 2018; WHO, 2004
Stigma reduction interventions: Clay et al., 2020
Task-sharing: Patel, 2009; Kakuma et al., 2011
Community-based care: Thornicroft, Deb and Henderson, 2016
Digital technology: Fu et al., 2020; Naslund et al., 2017; Doraiswamy et al., 2019
Integration with primary healthcare: Esponda et al., 2020; Petersen et al., 2019
Research priorities: Collins et al., 2011
Cost-effectiveness: Disease Control Priorities Mental, Neurological, and Substance Use Disorders; Chisholm and Saxena, 2012; Founders Pledge, 2019; Charity Entrepreneurship, 2020
WHO guidance: WHO, 2008a; WHO, 2013b
References
80,000 Hours. How to make a difference with your career (no date). Available at: https://80000hours.org/ (Accessed: 8 December 2020).
80, 000 Hours. Our list of high-impact careers (2015). Available at: https://80000hours.org/career-reviews/ (Accessed: 8 December 2020).
About us | Time To Change (n.d.). Available at: https://www.time-to-change.org.uk/about-us (Accessed: 8 August 2020).
Accenture (2018) IT’S NOT 1 IN 4; IT’S ALL OF US. Why mental health touches everyone.
Adams, L. and Turk, D. (2015) ‘Psychosocial Factors and Central Sensitivity Syndromes’, Current Rheumatology Reviews. Bentham Science Publishers Ltd., 11(2), pp. 96–108. doi: 10.2174/1573397111666150619095330.
Amoroso, M. et al. (2019) ‘Intranasal Mycobacterium vaccae administration prevents stress-induced aggravation of dextran sulfate sodium (DSS) colitis’, Brain, Behavior, and Immunity. Academic Press Inc., 80, pp. 595–604. doi: 10.1016/j.bbi.2019.05.005.
Anderson, P., Chisholm, D. and Fuhr, D. C. (2009) ‘Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol’, The Lancet. Lancet, pp. 2234–2246. doi: 10.1016/S0140-6736(09)60744-3.
Andrade, L. H. et al. (2014) ‘Barriers to mental health treatment: Results from the WHO World Mental Health surveys’, Psychological Medicine. Cambridge University Press, 44(6), pp. 1303–1317. doi: 10.1017/S0033291713001943.
Andrews, G. et al. (2010) ‘Computer Therapy for the Anxiety and Depressive Disorders Is Effective, Acceptable and Practical healthcare: A Meta-Analysis’, PLoS ONE. Edited by B. T. Baune. Public Library of Science, 5(10), p. e13196. doi: 10.1371/journal.pone.0013196.
Arjadi, R. and Patel, V. (2018) ‘Q&A: Scaling up delivery of mental health treatments in low and middle income countries: Interviews with Retha Arjadi and Vikram Patel’, BMC Medicine. BioMed Central Ltd., p. 211. doi: 10.1186/s12916-018-1209-1.
Bachmann S. Epidemiology of Suicide and the Psychiatric Perspective. Int J Environ Res Public Health. 2018 Jul 6;15(7):1425. doi: 10.3390/ijerph15071425. PMID: 29986446; PMCID: PMC6068947.
Bair, M. J. et al. (2003) ‘Depression and Pain Comorbidity: A Literature Review’, Archives of Internal Medicine. American Medical Association, pp. 2433–2445. doi: 10.1001/archinte.163.20.2433.
Barbui, C. et al. (2020) ‘Efficacy of psychosocial interventions for mental health outcomes in low-income and middle-income countries: an umbrella review’, The Lancet Psychiatry. Elsevier Ltd, 7(2), pp. 162–172. doi: 10.1016/S2215-0366(19)30511-5.
Bauer, M. S. et al. (2015) ‘An introduction to implementation science for the non-specialist’, BMC Psychology. BioMed Central Ltd., 3(1), pp. 1–12. doi: 10.1186/S40359-015-0089-9.
Beeharry G, Chambers D, Whiteford HA, Baingana F. Outlining the Scope for Public Sector Involvement in Mental Health. 2002.
Beidas, R. S. and Kendall, P. C. (2010) ‘Training therapists in evidence-based practice: A critical review of studies from a systems-contextual perspective’, Clinical Psychology: Science and Practice. John Wiley & Sons, Ltd, 17(1), pp. 1–30. doi: 10.1111/j.1468-2850.2009.01187.x.
Beidas, R. S. et al. (2019) ‘A repeated cross-sectional study of clinicians’ use of psychotherapy techniques during 5 years of a system-wide effort to implement evidence-based practices in Philadelphia’, Implementation Science. BioMed Central Ltd., 14(1), pp. 1–13. doi: 10.1186/s13012-019-0912-4.
Bickman, L. (2020) ‘Improving Mental Health Services: A 50-Year Journey from Randomized Experiments to Artificial Intelligence and Precision Mental Health’, Administration and Policy in Mental Health and Mental Health Services Research. Springer, 47(5), pp. 795–843. doi: 10.1007/s10488-020-01065-8.
Bilbo, S. D. and Schwarz, J. M. (2012) ‘The immune system and developmental programming of brain and behavior’, Frontiers in Neuroendocrinology. NIH Public Access, pp. 267–286. doi: 10.1016/j.yfrne.2012.08.006.
Birkjaer Micah Kaats Alejandro Rubio, M. et al. (2020) Wellbeing Adjusted Life Years A universal metric to quantify the happiness return on investment. Happiness Research Institute.
Blas, E, Sivasankara Kurup, A & World Health Organization. (2010). Equity, social determinants and public health programmes / editors Erik Blas and Anand Sivasankara Kurup. World Health Organization. https://apps.who.int/iris/handle/10665/44289
Bloom, D.E., Cafiero, E.T., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L.R., Fathima, S., Feigl, A.B., Gaziano, T., Mowafi, M., Pandya, A., Prettner, K., Rosenberg, L., Seligman, B., Stein, A.Z., & Weinstein, C. (2011). The Global Economic Burden of Noncommunicable Diseases. Geneva: World Economic Forum.
Bogenschutz, M. P. et al. (2015) ‘Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study’, Journal of Psychopharmacology. SAGE Publications Ltd, 29(3), pp. 289–299. doi: 10.1177/0269881114565144.
Brunoni, A. R. et al. (2017) ‘Repetitive transcranial magnetic stimulation for the acute treatment of major depressive episodes a systematic review with network meta-analysis’, JAMA Psychiatry. American Medical Association, pp. 143–152. doi: 10.1001/jamapsychiatry.2016.3644.
Burgess, R. A. et al. (2020) ‘Social interventions: a new era for global mental health?’, The Lancet Psychiatry. Elsevier Ltd, pp. 118–119. doi: 10.1016/S2215-0366(19)30397-9.
Cahill, H. and Romei, K. (2019) Melbourne Graduate School of Education PREVENTING GENDER-BASED VIOLENCE IN SCHOOLS IN EAST AND SOUTHERN AFRICA: FROM CONSULTATION TO CAPACITY BUILDING.
Capriati M, Hillebrandt H. Against Malaria Foundation· Giving What We Can. 2016. Available from: https://www.givingwhatwecan.org/report/against-malaria-foundation/
Caspi, A. et al. (2014) ‘The p factor: One general psychopathology factor in the structure of psychiatric disorders?’, Clinical Psychological Science. SAGE Publications Inc., 2(2), pp. 119–137. doi: 10.1177/2167702613497473.
Catrina Stewart. Chained, flogged and starved: report reveals ‘unimaginable’ treatment of Nigeria’s mentally ill. (2019). Available at: https://www.telegraph.co.uk/global-health/climate-and-people/chained-flogged-starved-report-reveals-unimaginable-treatment/ (Accessed: 8 August 2020).
Chains of love: the shocking reality of Cambodia’s mental healthcare | The Independent (2020). Available at: https://www.independent.co.uk/news/long_reads/health-and-wellbeing/cambodia-mentally-ill-chained-locked-khmer-rouge-a9351416.html (Accessed: 8 August 2020).
Charlson, F. J. et al. (2015) ‘Excess mortality from mental, neurological and substance use disorders in the Global Burden of Disease Study 2010’, Epidemiology and Psychiatric Sciences. Cambridge University Press, 24(2), pp. 121–140. doi: 10.1017/S2045796014000687.
Charlson, F. J. et al. (2016) ‘Excess mortality from mental, neurological and substance use disorders in the Global Burden of Disease Study 2010 Corrigendum’, Epidemiology and Psychiatric Sciences. Cambridge University Press, pp. 91–92. doi: 10.1017/S2045796015000724.
Charlson, F. J. et al. (2017) ‘Donor Financing of Global Mental Health, 1995—2015: An Assessment of Trends, Channels, and Alignment with the Disease Burden’, PLOS ONE. Edited by P. K. Maulik. Public Library of Science, 12(1), p. e0169384. doi: 10.1371/journal.pone.0169384.
Charlson, F. et al. (2019) ‘New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis’, The Lancet. Lancet Publishing Group, 394(10194), pp. 240–248. doi: 10.1016/S0140-6736(19)30934-1.
Chibanda, D. (2016) Five promising mental health interventions in low and middle income countries, Wellcome Trust. Available at: https://wellcome.ac.uk/news/five-promising-mental-health-interventions-low-and-middle-income-countries (Accessed: 8 August 2020).
Chisholm, D. et al. (2016b) ‘Scaling-up treatment of depression and anxiety: A global return on investment analysis’, The Lancet Psychiatry. Elsevier Ltd, 3(5), pp. 415–424. doi: 10.1016/S2215-0366(16)30024-4.
Chisholm, D., Johansson, K. A., et al. (2016a) ‘Universal Health Coverage for Mental, Neurological, and Substance Use Disorders: An Extended Cost-Effectiveness Analysis’, in Disease Control Priorities, Third Edition (Volume 4): Mental, Neurological, and Substance Use Disorders. The World Bank, pp. 237–251. doi: 10.1596/978-1-4648-0426-7_ch13.
Chisholm, D., Lund, C. and Saxena, S. (2007) ‘Cost of scaling up mental healthcare in low- and middle-income countries’, British Journal of Psychiatry. Br J Psychiatry, 191(DEC.), pp. 528–535. doi: 10.1192/bjp.bp.107.038463.
Chisholm, D. and Saxena, S. (2012) ‘Cost effectiveness of strategies to combat neuropsychiatric conditions in sub-Saharan Africa and South East Asia: mathematical modelling study.’, BMJ (Clinical research ed.). British Medical Journal Publishing Group, 344. doi: 10.1136/bmj.e609.
Cho, S. M. and Shin, Y. M. (2013) ‘The promotion of mental health and the prevention of mental health problems in child and adolescent’, Korean Journal of Pediatrics. Korean Pediatric Society, pp. 459–464. doi: 10.3345/kjp.2013.56.11.459.
Christensen, H., Griffiths, K. M. and Farrer, L. (2009) ‘Adherence in internet interventions for anxiety and depression’, Journal of Medical Internet Research. Journal of Medical Internet Research, p. e13. doi: 10.2196/jmir.1194.
Clark, A. E. et al. (2017) World Happiness Report Chapter 5: THE KEY DETERMINANTS OF HAPPINESS AND MISERY. World Happiness Report.
Clay, Jennifer et al. (2020) ‘Core components of mental health stigma reduction interventions in low-and middle-income countries: a systematic review’, Epidemiology and Psychiatric Sciences, 29(e164), pp. 1–16. doi: 10.1017/S2045796020000797.
Collins, P. Y. and Saxena, S. (2016) ‘Action on mental health needs global cooperation’, Nature. Nature Publishing Group, pp. 25–27. doi: 10.1038/532025.
Collins, P. Y. et al. (2011) ‘Grand challenges in global mental health’, Nature. Nature Publishing Group, 475(7354), pp. 27–30. doi: 10.1038/475027a.
Collins, P. Y. et al. (2013) ‘Grand Challenges in Global Mental Health: Integration in Research, Policy, and Practice’, PLoS Medicine. Public Library of Science, 10(4), p. e1001434. doi: 10.1371/journal.pmed.1001434.
Corrigan, P. W. and Watson, A. C. (2002) ‘Understanding the impact of stigma on people with mental illness.’, World psychiatry : official journal of the World Psychiatric Association (WPA). World Psychiatric Association, 1(1), pp. 16–20. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16946807 (Accessed: 8 August 2020).
Cuijpers P, Turner EH, Mohr DC, Hofmann SG, Andersson G, Berking M, Coyne J. Comparison of psychotherapies for adult depression to pill placebo control groups: a meta-analysis. Psychol Med. 2014 Mar;44(4):685-95. doi: 10.1017/S0033291713000457. Epub 2013 Apr 3. PMID: 23552610.
Das-Munshi, J. et al. (2008) ‘Public health significance of mixed anxiety and depression: Beyond current classification’, British Journal of Psychiatry. Br J Psychiatry, 192(3), pp. 171–177. doi: 10.1192/bjp.bp.107.036707.
Deb, K. and Gupta, S. (2017) ‘Prevention strategies for substance use disorders in low-resource settings’, Indian Journal of Social Psychiatry. Medknow, 33(2), p. 112. doi: 10.4103/ijsp.ijsp_41_17.
DeRubeis, R. J. (2019) ‘The history, current status, and possible future of precision mental health’, Behaviour Research and Therapy. Elsevier Ltd, 123, p. 103506. doi: 10.1016/j.brat.2019.103506.
Dieleman, J. L. et al. (2014) ‘Global Health Development Assistance Remained Steady In 2013 But Did Not Align With Recipients’ Disease Burden’, Health Affairs. Project HOPE, 33(5), pp. 878–886. doi: 10.1377/hlthaff.2013.1432.
Dias, M. & Fontes, L., (2020) “The Effects of a Large-Scale Mental-Health Reform: Evidence from Brazil,” MPRA Paper 104753, University Library of Munich, Germany.
Dolan, P. and Kahneman, D. (2008) ‘Interpretations of utility and their implications for the valuation of health’, Economic Journal. John Wiley & Sons, Ltd, 118(525), pp. 215–234. doi: 10.1111/j.1468-0297.2007.02110.x.
Doraiswamy, P. M. et al. (2019) ‘Empowering 8 Billion Minds: Enabling Better Mental Health for All via the Ethical Adoption of Technologies’, NAM Perspectives. National Academy of Medicine. doi: 10.31478/201910b.
Drew, N. et al. (2011) ‘Human rights violations of people with mental and psychosocial disabilities: An unresolved global crisis’, The Lancet. Elsevier, pp. 1664–1675. doi: 10.1016/S0140-6736(11)61458-X.
Dudley, M., Silove, D. and Gale, F. (eds) (2012) Mental Health and Human Rights: Vision, Praxis, and Courage – Google Books. Oxford: OUP.
Elizabeth (2017) Mental Health Shallow Review – EA Forum. Available at: https://forum.effectivealtruism.org/posts/if24DY4pW2FZPPT4G/mental-health-shallow-review (Accessed: 26 November 2020).
Esponda, G. M. et al. (2020) ‘Barriers and facilitators of mental health programmes in primary care in low-income and middle-income countries’, The Lancet Psychiatry. Elsevier Ltd, pp. 78–92. doi: 10.1016/S2215-0366(19)30125-7.
Ferrari, A. J. et al. (2014) ‘The burden attributable to mental and substance use disorders as risk factors for suicide: Findings from the Global Burden of Disease Study 2010’, PLoS ONE. Public Library of Science, 9(4). doi: 10.1371/journal.pone.0091936.
Firth, J. et al. (2017) ‘The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials’, World Psychiatry. Blackwell Publishing Ltd, 16(3), pp. 287–298. doi: 10.1002/wps.20472.
Ganju, A. et al. (2020) ‘Systemic solutions for addressing non-communicable diseases in low-and middle-income countries’, Journal of Multidisciplinary Healthcare. Dove Medical Press Ltd., pp. 693–707. doi: 10.2147/JMDH.S252300.
Garnett, G. P. et al. (2017) Cost-Effectiveness of Interventions to Prevent HIV Acquisition.
Gates, K. et al. (2016) ‘You can’t treat what you don’t diagnose: An analysis of the recognition of somatic presentations of depression and anxiety in primary care’, Families, Systems and Health. American Psychological Association Inc., 34(4), pp. 317–329. doi: 10.1037/fsh0000229.
Gaudiano, B. A. (2008) ‘Cognitive-behavioural therapies: Achievements and challenges’, Evidence-Based Mental Health. NIH Public Access, pp. 5–7. doi: 10.1136/ebmh.11.1.5.
GBD Compare | IHME Viz Hub (n.d.). Available at: https://vizhub.healthdata.org/gbd-compare/ (Accessed: 8 August 2020).
GBD Results Tool | GHDx (n.d.). Available at: http://ghdx.healthdata.org/gbd-results-tool (Accessed: 8 August 2020).
Gilbert, D. T. and Wilson, T. D. (2007) ‘Prospection: Experiencing the future’, Science, 317(5843), pp. 1351–1354. doi: 10.1126/science.1144161.
GiveWell’s Cost-Effectiveness Analyses | GiveWell [Internet]. 2020 [cited 2020 Oct 16]. Available from: https://www.givewell.org/how-we-work/our-criteria/cost-effectiveness/cost-effectiveness-models
Global Advocacy Team (2012) Learn Without Fear: The campaign to stop violence in schools. Third progress report . Woking. Plan International. Available at: https://plan-international.org/publications/learn-without-fear-third-progress-report (Accessed: 8 August 2020).
Goodman, S. H. (2020) ‘Intergenerational Transmission of Depression’, Annual Review of Clinical Psychology. Annual Reviews Inc., 16(1), pp. 213–238. doi: 10.1146/annurev-clinpsy-071519-113915.
Goth A, Hoeijmakers S. (2020) Charity Recommendation Report: Action for Happiness. Founders Pledge. doi: 10.1257/aer.103.3.598.
Goth, A. and Hoeijmakers, S. (2020) Psychedelic-Assisted Mental Health Treatments Cause Area Report. Founders Pledge.
Gorringe et al., (2020) THE RETURN ON THE INDIVIDUAL: TIME TO INVEST IN MENTAL HEALTH ABOUT SPEAK YOUR MIND AND THE ROI REPORT James Sale Policy and Advocacy Manager, United for Global Mental Health.
Griffiths, R. R. et al. (2016) ‘Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial’, Journal of Psychopharmacology. SAGE Publications Ltd, 30(12), pp. 1181–1197. doi: 10.1177/0269881116675513.
Hansen, B. et al. (2018) ‘The Bergen 4-day OCD treatment delivered in a group setting: 12-month follow-up’, Frontiers in Psychology. Frontiers Media S.A., 9(MAY), p. 639. doi: 10.3389/fpsyg.2018.00639.
Harvey, A. G. et al. (2014) ‘Improving Outcome of Psychosocial Treatments by Enhancing Memory and Learning’, Perspectives on Psychological Science. NIH Public Access, 9(2), pp. 161–179. doi: 10.1177/1745691614521781.
Headspace. Researching Meditation and Mindfulness [Internet]. 2020 [cited 2020 Dec 13]. Available from: https://www.headspace.com/science/meditation-research
Hidaka, B. H. (2012) ‘Depression as a disease of modernity: Explanations for increasing prevalence’, Journal of Affective Disorders. NIH Public Access, pp. 205–214. doi: 10.1016/j.jad.2011.12.036.
Hofmann, S. G. et al. (2012) ‘The efficacy of cognitive behavioral therapy: A review of meta-analyses’, Cognitive Therapy and Research. Springer New York LLC, pp. 427–440. doi: 10.1007/s10608-012-9476-1.
Horton, S. (2016) Cost-Effectiveness Analysis in Disease Control Priorities, Third Edition.
Human Rights Watch. LIVING IN HELL Abuses against People with Psychosocial Disabilities in Indonesia (2016).
Killaspy, H. (2006) ‘From the asylum to community care: learning from experience’, British Medical Bulletin. Oxford Academic, 79–80(1), pp. 245–258. doi: 10.1093/bmb/ldl017.
Kocsis JH, Leon AC, Markowitz JC, Manber R, Arnow B, Klein DN, et al. Patient preference as a moderator of outcome for chronic forms of major depressive disorder treated with nefazodone, cognitive behavioral analysis system of psychotherapy, or their combination. J Clin Psychiatry [Internet]. 2009 Mar [cited 2020 Sep 30];70(3):354–61. Available from: https://pubmed.ncbi.nlm.nih.gov/19192474/
Global Citizen (2017) In West Africa, Mental Illness Is Treated With Chains & Shackles. Available at: https://www.globalcitizen.org/fr/content/the-places-where-mental-illness-is-treated-with-ch/ (Accessed: 8 August 2020).
Institute for Health Metrics and Evaluation (IHME). About GBD (n.d.). Available at: http://www.healthdata.org/gbd/about (Accessed: 8 August 2020).
IHME. Protocol for the global burden of diseases, injuries, and risk factors study (GBD) (2020). Available at: http://www.healthdata.org/sites/default/files/files/Projects/GBD/March2020_GBD Protocol_v4.pdf (Accessed: 8 August 2020).
Jasanoff, A. (2018) The Biological Mind: How Brain, Body, and Environment… – Google Scholar. Basic Books.
Jenkins, R. et al. (2010) ‘International Migration of Doctors, and Its Impact on Availability of Psychiatrists in Low and Middle Income Countries’, PLoS ONE. Edited by P. J. Hay. Public Library of Science, 5(2), p. e9049. doi: 10.1371/journal.pone.0009049.
Johnson, M. W., Garcia-Romeu, A. and Griffiths, R. R. (2017) ‘Long-term follow-up of psilocybin-facilitated smoking cessation’, American Journal of Drug and Alcohol Abuse. Taylor and Francis Ltd, 43(1), pp. 55–60. doi: 10.3109/00952990.2016.1170135.
Kakuma, R. et al. (2011) ‘Human resources for mental healthcare: Current situation and strategies for action’, The Lancet. Elsevier, pp. 1654–1663. doi: 10.1016/S0140-6736(11)61093-3.
Kapfhammer, H. P. (2006) ‘Somatic symptoms in depression’, Dialogues in Clinical Neuroscience. Les Laboratoires Servier, pp. 227–239. doi: 10.1016/s0924-9338(99)80453-2.
Karimi, M., Brazier, J. and Paisley, S. (2017) ‘Are preferences over health states informed?’, Health and Quality of Life Outcomes. BioMed Central Ltd., 15(1), p. 105. doi: 10.1186/s12955-017-0678-9.
Kermode, M. et al. (2011) ‘Opioid substitution therapy in resource-poor settings’, Bulletin of the World Health Organization, p. 243. doi: 10.2471/BLT.11.086850.
Knaak, S., Mantler, E. and Szeto, A. (2017) ‘Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions’, Healthcare Management Forum. SAGE Publications Inc., pp. 111–116. doi: 10.1177/0840470416679413.
Knaak, S., Ungar, T. and Patten, S. (2015) ‘Seeing is believing: Biological information may reduce mental health stigma amongst physicians’, Australian and New Zealand Journal of Psychiatry. Taylor and Francis Ltd, pp. 751–752. doi: 10.1177/0004867415584643.
Knapp, M., Mcdaid, D. and Parsonage, M. (2011) Mental health promotion and mental illness prevention: The economic case.
Knapp, M. and Wong, G. (2020) ‘Economics and mental health: the current scenario’, World Psychiatry. Blackwell Publishing Ltd, 19(1), pp. 3–14. doi: 10.1002/wps.20692.
Kvaale, E. P., Haslam, N. and Gottdiener, W. H. (2013) ‘The “side effects” of medicalization: A meta-analytic review of how biogenetic explanations affect stigma’, Clinical Psychology Review. Pergamon, pp. 782–794. doi: 10.1016/j.cpr.2013.06.002.
Leach-Kemon, K. et al. (2013) ‘Filling gaps in all-cause and cause-specific mortality and disability data are essential for improving Global Burden of Disease estimation: descriptive study of missing data by country and region’, The Lancet. Elsevier BV, 381, p. S82. doi: 10.1016/s0140-6736(13)61336-7.
Lee, S. (2009) ‘Mental illness in China’, The Lancet. Elsevier, pp. 1063–1064. doi: 10.1016/S0140-6736(09)61699-8.
Levin, C., Chisholm, D. , . “Cost-Effectiveness and Affordability of Interventions, Policies, and Platforms for the Prevention and Treatment of Mental, Neurological and Substance Use Disorders ”. In: Disease Control Priorities (third edition): Volume 4, Mental, Neurological, and Substance Use Disorders, edited by V. Patel, D. Chisholm, T. Dua, R. Laxminarayan, M. Medina. Washington, DC: World Bank.
Liese, B. H., Gribble, R. S. F. and Wickremsinhe, M. N. (2019) ‘International funding for mental health: a review of the last decade’. doi: 10.1093/inthealth/ihz040.
Lopez-Munoz, F. and Alamo, C. (2009) ‘Monoaminergic Neurotransmission: The History of the Discovery of Antidepressants from 1950s Until Today’, Current Pharmaceutical Design. Bentham Science Publishers Ltd., 15(14), pp. 1563–1586. doi: 10.2174/138161209788168001.
Lund, C. et al. (2018) ‘Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews’, The Lancet Psychiatry. Elsevier Ltd, pp. 357–369. doi: 10.1016/S2215-0366(18)30060-9.
Lund, C. (2019) ‘Reflections on the next ten years of research, policy and implementation in global mental health’, Epidemiology and psychiatric sciences. NLM (Medline), 29, p. e77. doi: 10.1017/S204579601900074X.
Lund, C. et al. (2020) ‘Task-sharing of psychological treatment for antenatal depression in Khayelitsha, South Africa: Effects on antenatal and postnatal outcomes in an individual randomised controlled trial’, Behaviour Research and Therapy. Elsevier Ltd, 130, p. 103466. doi: 10.1016/j.brat.2019.103466.
Making the Investment Case for Mental Health: A WHO / UNDP Methodological Guidance Note (2019). Available at: http://apps.who.int/bookorders. (Accessed: 29 May 2020).
Mascayano, F., Armijo, J. E. and Yang, L. H. (2015) ‘Addressing stigma relating to mental illness in low- and middle-income countries’, Frontiers in Psychiatry. Frontiers Media S.A., 6(MAR). doi: 10.3389/fpsyt.2015.00038.
Maulik, P. K., Thornicroft, G. and Saxena, S. (2020) ‘Roadmap to strengthen global mental health systems to tackle the impact of the COVID-19 pandemic’, International Journal of Mental Health Systems. BioMed Central, p. 57. doi: 10.1186/s13033-020-00393-4.
McAleavey, A. A. et al. (2019) ‘Effectiveness of routine psychotherapy: Method matters’, Psychotherapy Research. Routledge, 29(2), pp. 139–156. doi: 10.1080/10503307.2017.1395921.
McCloskey, L. A. et al. (2016) ‘Determinants of Intimate Partner Violence in Sub-Saharan Africa: A Review of Prevention and Intervention Programs’, Partner Abuse. Springer Publishing Company, 7(3), pp. 277–315. doi: 10.1891/1946-6560.7.3.277.
Melville KM, Casey LM, Kavanagh DJ. Dropout from Internet-based treatment for psychological disorders. Br J Clin Psychol. 2010 Nov;49(Pt 4):455-71. doi: 10.1348/014466509X472138. Epub 2009 Oct 1. PMID: 19799804.
Mental Health Atlas (2005).
Mental health programme evaluation – HAPPIER LIVES INSTITUTE (2020). Available at: https://www.happierlivesinstitute.org/report/mental-health-programme-evaluation-project/ (Accessed: 28 September 2020).
MENTAL HEALTH USERS NETWORK OF ZAMBIA (MHUNZA) – Idealist (2003). Available at: https://www.idealist.org/en/nonprofit/dd7f41c3ccd84dddb6737d0878db6bda-mental-health-users-network-of-zambiamh-lusaka (Accessed: 28 September 2020).
Mentally ill patients in Indonesia held in chains – BBC News (2013a). Available at: https://www.bbc.co.uk/news/health-22076563 (Accessed: 8 August 2020).
Merikangas, K. R. and Merikangas, A. K. (2019) ‘Harnessing progress in psychiatric genetics to advance population mental health’, American Journal of Public Health. American Public Health Association Inc., pp. S171–S175. doi: 10.2105/AJPH.2019.304948.
Meyer, A. C. et al. (2010) ‘Global disparities in the epilepsy treatment gap: A systematic review’, Bulletin of the World Health Organization, 88(4), pp. 260–266. doi: 10.2471/BLT.09.064147.
Mithoefer, M. C. et al. (2019) ‘MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials’, Psychopharmacology. Springer Verlag, 236(9), pp. 2735–2745. doi: 10.1007/s00213-019-05249-5.
Moffitt, T. E. et al. (2007) ‘Depression and generalized anxiety disorder: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years’, Archives of General Psychiatry. Arch Gen Psychiatry, 64(6), pp. 651–660. doi: 10.1001/archpsyc.64.6.651.
Moreno, F. A. et al. (2006) ‘Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder’, Journal of Clinical Psychiatry. Physicians Postgraduate Press Inc., 67(11), pp. 1735–1740. doi: 10.4088/JCP.v67n1110.
Mulder, R. T., Scott, K. M. and Jorm, A. F. (2020) ‘Making sense of the vulnerability paradox in cross-national studies of mental disorders: Lessons from research on subjective well-being’, Australian and New Zealand Journal of Psychiatry. SAGE Publications Inc., pp. 664–666. doi: 10.1177/0004867420927464.
Nadkarni, A. et al. (2017) ‘Counselling for Alcohol Problems (CAP), a lay counsellor-delivered brief psychological treatment for harmful drinking in men, in primary care in India: a randomised controlled trial’, The Lancet. Lancet Publishing Group, 389(10065), pp. 186–195. doi: 10.1016/S0140-6736(16)31590-2.
Naslund, J. A. et al. (2017) ‘Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature’, The Lancet Psychiatry. Elsevier Ltd, pp. 486–500. doi: 10.1016/S2215-0366(17)30096-2.
National Institute on Drug Abuse (NIDA). Comorbidity: Substance Use Disorders and Other Mental Illnesses DrugFacts (2018). Available at: https://www.drugabuse.gov/publications/drugfacts/comorbidity-substance-use-disorders-other-mental-illnesses (Accessed: 8 August 2020).
NEUROLOGICAL DISORDERS public health challenges WHO Library Cataloguing-in-Publication Data (2006).
NICE (2019) Guidance | Generalised anxiety disorder and panic disorder in adults: management . Available at: https://www.nice.org.uk/guidance/cg113/chapter/1-Guidance#principles-of-care-for-people-with-generalised-anxiety-disorder-gad (Accessed: 8 August 2020).
Nordmo, M. et al. (2020) ‘Effectiveness of Open-Ended Psychotherapy Under Clinically Representative Conditions’, Frontiers in Psychiatry. Frontiers Media S.A., 11, p. 384. doi: 10.3389/fpsyt.2020.00384.
Patel, V. et al. (2007) ‘Treatment and prevention of mental disorders in low-income and middle-income countries’, Lancet. Elsevier, pp. 991–1005. doi: 10.1016/S0140-6736(07)61240-9.
Patel, V. (2009) ‘The future of psychiatry in low- and middle-income countries.’, Psychological medicine, 39(11), pp. 1759–62. doi: 10.1017/s0033291709005224.
Patel, V. et al. (2016a) ‘Addressing the burden of mental, neurological, and substance use disorders: Key messages from Disease Control Priorities, 3rd edition’, The Lancet. Lancet Publishing Group, pp. 1672–1685. doi: 10.1016/S0140-6736(15)00390-6.
Patel, V. et al. (2017) ‘The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial’, The Lancet. Lancet Publishing Group, 389(10065), pp. 176–185. doi: 10.1016/S0140-6736(16)31589-6.
Patel, V. et al. (2018) ‘The Lancet Commissions The Lancet Commission on global mental health and sustainable development Executive summary’, The Lancet, 392, pp. 1553–1598. doi: 10.1016/S0140-6736(18)31612-X.
Patel, V. and Chatterji, S. (2015) ‘Integrating mental health in care for noncommunicable diseases: An imperative for person-centered care’, Health Affairs. Project HOPE, 34(9), pp. 1498–1505. doi: 10.1377/hlthaff.2015.0791.
Patel, V. and Saxena, S. (2014) ‘Transforming Lives, Enhancing Communities — Innovations in Global Mental Health’, New England Journal of Medicine. Massachusetts Medical Society, 370(6), pp. 498–501. doi: 10.1056/NEJMp1315214.
Peasgood, T., Foster, D. and Dolan, P. (2019) Global Happiness and Wellbeing Policy Report 2019 Chapter 3: Priority Setting in Healthcare Through the Lens of Happiness.
Petersen, I. et al. (2019) ‘Scaling up integrated primary mental health in six low- and middle-income countries: obstacles, synergies and implications for systems reform’, BJPsych Open. Royal College of Psychiatrists, 5(5). doi: 10.1192/bjo.2019.7.
Phillips, M. R. et al. (2009) ‘Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey’, The Lancet. Lancet, 373(9680), pp. 2041–2053. doi: 10.1016/S0140-6736(09)60660-7.
Plana-Ripoll, O. et al. (2019) ‘Exploring Comorbidity Within Mental Disorders among a Danish National Population’, JAMA Psychiatry. American Medical Association, 76(3), pp. 259–270. doi: 10.1001/jamapsychiatry.2018.3658.
Plant, M. (2018) Cause profile: mental health – EA Forum. Available at: https://forum.effectivealtruism.org/posts/XWSTBBH8gSjiaNiy7/cause-profile-mental-health (Accessed: 26 November 2020)
Plant, Michael (2019). _Doing Good Badly? Philosophical Issues Related to Effective Altruism_. Dissertation, Oxford University
Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health. 2009 Jan;36(1):24-34. doi: 10.1007/s10488-008-0197-4. Epub 2008 Dec 23. PMID: 19104929; PMCID: PMC3808121.
Public Health England (PHE). Commissioning Cost-Effective Services for Promotion of Mental Health and Wellbeing and Prevention of Mental Ill-Health (2017). Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/640714/Commissioning_effective_mental_health_prevention_report.pdf (Accessed: 8 August 2020).
Pyne, J. M. et al. (2009) ‘How Bad Is Depression? Preference Score Estimates from Depressed Patients and the General Population’, Health Services Research. John Wiley & Sons, Ltd, 44(4), pp. 1406–1423. doi: 10.1111/j.1475-6773.2009.00974.x.
Rasmussen, J. D. et al. (2019) ‘Portrayals of mental illness, treatment, and relapse and their effects on the stigma of mental illness: Population-based, randomized survey experiment in rural Uganda’, PLoS Medicine. Public Library of Science, p. e1002908. doi: 10.1371/journal.pmed.1002908.
Reuben, A. et al. (2019) ‘Association of childhood lead exposure with adult personality traits and lifelong mental health’, JAMA Psychiatry. American Medical Association, 76(4), pp. 418–425. doi: 10.1001/jamapsychiatry.2018.4192.
Reynolds, A. J. et al. (2007) ‘Effects of a school-based, early childhood intervention on adult health and well-being: A 19-year follow-up of low-income families’, Archives of Pediatrics and Adolescent Medicine. American Medical Association, 161(8), pp. 730–739. doi: 10.1001/archpedi.161.8.730.
Ridley, M. et al. (2020) “Poverty, Depression, and Anxiety: Causal Evidence and Mechanisms.” Science, 370(6522). doi: 10.1126/science.aay0214.
Rogers, A. (2017) Star Neuroscientist Tom Insel Leaves the Google-Spawned Verily for … a Startup? | WIRED, Wired. Available at: https://www.wired.com/2017/05/star-neuroscientist-tom-insel-leaves-google-spawned-verily-startup/ (Accessed: 18 May 2021).
Rose-Clarke K, Gurung D, Brooke-Sumner C, Burgess R, Burns J, Kakuma R, et al. Rethinking research on the social determinants of global mental health. Vol. 7, The Lancet Psychiatry. Elsevier Ltd; 2020. p. 659–62
Ruggiero, G. M. et al. (2018) ‘A Historical and Theoretical Review of Cognitive Behavioral Therapies: From Structural Self-Knowledge to Functional Processes’, Journal of Rational – Emotive and Cognitive – Behavior Therapy. Springer New York LLC, 36(4), pp. 378–403. doi: 10.1007/s10942-018-0292-8.
Ruscio AM. Normal Versus Pathological Mood: Implications for Diagnosis. Annu Rev Clin Psychol. 2019 May 7;15:179-205. doi: 10.1146/annurev-clinpsy-050718-095644. PMID: 31067413.
Sangath (n.d.). Available at: https://www.sangath.in/ (Accessed: 28 September 2020).
Saraceno, B. et al. (2007) ‘Barriers to improvement of mental health services in low-income and middle-income countries’, Lancet. Elsevier, pp. 1164–1174. doi: 10.1016/S0140-6736(07)61263-X.
Sartorius, Norman & WHO Collaborative Study on Standardized Assessment of Depressive Disorders. (1983). Depressive disorders in different cultures : report on the WHO Collaborative Study on Standardized Assessment of Depressive Disorders / N. Sartorius … [et al.]. World Health Organization. https://apps.who.int/iris/handle/10665/37139
Saxena, S. et al. (2007) ‘Resources for mental health: scarcity, inequity, and inefficiency’, Lancet. Elsevier, pp. 878–889. doi: 10.1016/S0140-6736(07)61239-2.
Saxena, S. et al. (2019) ‘Countdown Global Mental Health 2030’, The Lancet. Lancet Publishing Group, pp. 858–859. doi: 10.1016/S0140-6736(19)30424-6.
Saxena S, Sharan P, Garrido M, Saraceno B. World Health Organization’s Mental Health Atlas 2005:implications for policy development. World Psychiatry [Internet]. 2006 Oct [cited 2020 Oct 14];5(3):179–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17139355
Saxena, S., Sharan, P. and Saraceno, B. (2003) ‘Budget and financing of mental health services: Baseline information on 89 countries from WHO’s Project Atlas’, Journal of Mental Health Policy and Economics, 6(3), pp. 135–143.
Scott, K. M. et al. (eds) (2018) Mental disorders around world facts and figures who world mental health surveys. Available at: https://www.cambridge.org/gb/academic/subjects/medicine/mental-health-psychiatry-and-clinical-psychology/mental-disorders-around-world-facts-and-figures-who-world-mental-health-surveys?format=HB (Accessed: 8 August 2020).
Shantna, K. et al. (2009) ‘Comorbid psychiatric disorders in substance dependence patients: A control study’, Industrial Psychiatry Journal. Medknow, 18(2), p. 84. doi: 10.4103/0972-6748.62265.
Smoller, J. W. (2017) ‘A Quarter Century of Progress in Psychiatric Genetics’, Harvard review of psychiatry. NIH Public Access, 25(6), pp. 256–258. doi: 10.1097/HRP.0000000000000180.
Snowden, J. and Halstead, J. (2019) Mental Health Cause Area Report. Founders Pledge.
Stein, D. J. et al. (2019) ‘Integrating mental health with other non-communicable diseases’, BMJ (Online). BMJ Publishing Group, 364. doi: 10.1136/bmj.l295.
Stigma and discrimination | Mental Health Foundation (2015). Available at: https://www.mentalhealth.org.uk/a-to-z/s/stigma-and-discrimination (Accessed: 8 August 2020).
Stone, A. A. and Mackie, C. (eds) (2013) Subjective Well-Being Measuring Happiness, Suffering, and Other Dimensions of Experience. National Research Council. Available at: http://www.nap.edu. (Accessed: 28 September 2020).
Stone, M. H. (1990) The Fate of Borderline Patients: Successful Outcome and Psychiatric Practice . The Guilford Press. Available at: https://books.google.co.uk/books?hl=en&lr=&id=SJoLZedMFXkC&oi=fnd&pg=PA1&ots=BoJj-D9kd5&sig=3pgGq-2tqkvPVEKxHmtx8XdEocA&redir_esc=y#v=onepage&q&f=false (Accessed: 8 August 2020).
Stover J, Bollinger L, Walker N, Monasch R. Resource needs to support orphans and vulnerable children in sub-Saharan Africa. Health Policy Plan. 2007;22(1):21-27. doi:10.1093/heapol/czl033
StrongMinds (n.d.) Mental Health Africa | Treating Depression In Women | UGANDA. Available at: https://strongminds.org/ (Accessed: 11 August 2020).
Stuckler, D. et al. (2008) ‘WHO’s budgetary allocations and burden of disease: a comparative analysis’, The Lancet. Elsevier, 372(9649), pp. 1563–1569. doi: 10.1016/S0140-6736(08)61656-6.
Summers, M. R. and Nevin, R. L. (2017) ‘Stellate Ganglion Block in the Treatment of Post-traumatic Stress Disorder: A Review of Historical and Recent Literature’, Pain Practice. Blackwell Publishing Inc., pp. 546–553. doi: 10.1111/papr.12503.
Thakur, K. T. et al. (2016) Neurological Disorders.
Thornicroft, G. et al. (2017) ‘Undertreatment of people with major depressive disorder in 21 countries’, British Journal of Psychiatry. Royal College of Psychiatrists, pp. 119–124. doi: 10.1192/bjp.bp.116.188078.
Thornicroft, G., Deb, T. and Henderson, C. (2016) ‘Community mental healthcare worldwide: current status and further developments’, World Psychiatry. Blackwell Publishing Ltd, 15(3), pp. 276–286. doi: 10.1002/wps.20349.
Thornicroft, G. and Sunkel, C. (2020) ‘Announcing the Lancet Commission on stigma and discrimination in mental health’, The Lancet. Elsevier BV, 396(10262), pp. 1543–1544. doi: 10.1016/s0140-6736(20)32203-0.
Thornicroft, G. and Tansella, M. (2013) ‘The balanced care model: The case for both hospital- and community-based mental healthcare’, British Journal of Psychiatry. Cambridge University Press, pp. 246–248. doi: 10.1192/bjp.bp.112.111377.
Time to Change. Stigma Shout – Service user and carer experiences of stigma and discrimination (2008).
Todd, B. (2014) 80,000 HOURS – The best ways to help others with your career, compared. Available at: https://80000hours.org/career-guide/high-impact-jobs/#approach-4-direct-work (Accessed: 9 December 2020).
Tracy McVeigh. ‘All we can offer is the chain’: the scandal of Ghana’s shackled sick | Global development | The Guardian (2020). Available at: https://www.theguardian.com/global-development/2020/feb/03/all-we-can-offer-is-the-chain-the-scandal-of-ghanas-shackled-sick (Accessed: 8 August 2020).
Trades Union Congress (2017) Mental health and employment. Available at: https://www.tuc.org.uk/sites/default/files/Disability and employment.pdf (Accessed: 23 September 2020).
Trautmann, S., Rehm, J. and Wittchen, H. (2016) ‘The economic costs of mental disorders’, EMBO reports. EMBO, 17(9), pp. 1245–1249. doi: 10.15252/embr.201642951.
Vigo, D., Thornicroft, G. and Atun, R. (2016) ‘Estimating the true global burden of mental illness’, The Lancet Psychiatry. Elsevier Ltd, pp. 171–178. doi: 10.1016/S2215-0366(15)00505-2.
Vigo, D. et al. (2020) ‘Mental Health of Communities during the COVID-19 Pandemic’, Canadian Journal of Psychiatry. SAGE Publications Inc., pp. 681–687. doi: 10.1177/0706743720926676.
Vos, T. et al. (2016) ‘Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015’, The Lancet. Lancet Publishing Group, 388(10053), pp. 1545–1602. doi: 10.1016/S0140-6736(16)31678-6.
Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008 Jan 17;358(3):252-60. doi: 10.1056/NEJMsa065779. PMID: 18199864.
UW Implementation Science Resource Hub (no date) What is Implementation Science? Available at: https://impsciuw.org/implementation-science/learn/implementation-science-overview/ (Accessed: 18 May 2021).
Wang, P. S. et al. (2007) ‘Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys’, Lancet. Elsevier, 370(9590), pp. 841–850. doi: 10.1016/S0140-6736(07)61414-7.
Wasserman, D. et al. (2015) ‘School-based suicide prevention programmes: The SEYLE cluster-randomised, controlled trial’, The Lancet. Lancet Publishing Group, 385(9977), pp. 1536–1544. doi: 10.1016/S0140-6736(14)61213-7.
Whiteford, H. A. et al. (2015) ‘The Global Burden of Mental, Neurological and Substance Use Disorders: An Analysis from the Global Burden of Disease Study 2010’, PLOS ONE. Edited by G. Forloni. Public Library of Science, 10(2), p. e0116820. doi: 10.1371/journal.pone.0116820.
Whiteford, H. A. et al. (2016) ‘Global Burden of Mental, Neurological, and Substance Use Disorders: An Analysis from the Global Burden of Disease Study 2010’, in Disease Control Priorities, Third Edition (Volume 4): Mental, Neurological, and Substance Use Disorders. The World Bank, pp. 29–40. doi: 10.1596/978-1-4648-0426-7_ch2.
Whiteford, H. A., Ferrari, A. J. and Vos, T. (2016) ‘Challenges to estimating the true global burden of mental disorders’, The Lancet Psychiatry. Elsevier Ltd, pp. 402–403. doi: 10.1016/S2215-0366(16)30026-8.
Wainberg, M. L. et al. (2017) ‘Challenges and Opportunities in Global Mental Health: a Research-to-Practice Perspective’, Current Psychiatry Reports. Current Medicine Group LLC 1, p. 28. doi: 10.1007/s11920-017-0780-z.
Premature death among people with severe mental disorders (n.d.-b). Available at: https://www.who.int/mental_health/management/info_sheet.pdf (Accessed: 8 August 2020).
WHO (2001) ‘The World Health Report Chapter 4: Mental Health Policy and Service Provision’.
WHO (2002) ‘Prevention and Promotion in Mental Health’
WHO (2003) Investing in Mental Health. Available at: www.who.int/mental_health (Accessed: 8 August 2020).
WHO (2004) Neurological Disorders Atlas.
WHO (2004) Prevention of Mental Disorders EFFECTIVE INTERVENTIONS AND POLICY OPTIONS SUMMARY REPORT.
WHO (2005) IMPROVING ACCESS AND USE OF PSYCHOTROPIC MEDICINES Mental Health Policy and Service Guidance Package.
WHO (2007) Expert Opinion on Barriers and Facilitating Factors for the Implementation of Existing Mental Health Knowledge in Mental Health Services.
WHO (2008a) ‘WORLD HEALTH ORGANIZATION. mhGAP Intervention Guide.’, in on line, pp. 1–173.
WHO (2008b) mhGAP Mental Health Gap Action Programme.
WHO (2010a) A SITUATION ANALYSIS OF MENTAL HEALTH IN SOMALIA.
WHO (2013a) Building Back Better Sustainable Mental healthcare after Emergencies. Available at: www.who.int (Accessed: 8 August 2020).
WHO (2013b) MENTAL HEALTH ACTION PLAN 2013-2020 ’ .
WHO (2015a) EXCESS MORTALITY IN PERSONS WITH SEVERE MENTAL DISORDERS (2015). Geneva. Available at: https://www.who.int/mental_health/evidence/excess_mortality_meeting_report.pdf?ua=1 (Accessed: 10 December 2020).
WHO (2015b) Global Mental Health: How are we doing? Available at: https://www.who.int/mental_health/evidence/atlas/interactive_infographic_2015.pdf (Accessed: 8 August 2020).
WHO (2017) Depression and Other Common Mental Disorders Global Health Estimates.
WHO (2018) Mental health: strengthening our response. Available at: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (Accessed: 8 August 2020).
WHO (2019a) Mental disorders. Available at: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (Accessed: 8 August 2020).
WHO (2019c) Global Spending on Health: A World in Transition. Available at: http://apps.who.int/bookorders. (Accessed: 8 August 2020).
WHO (2019d) Psychiatrists and nurses (per 100 000 population). Available at: https://www.who.int/gho/mental_health/human_resources/psychiatrists_nurses/en/ (Accessed: 8 August 2020).
WHO (2019f) Draft menu of cost-effective interventions for mental health. Available at: https://www.who.int/mental_health/WHO_Discussion_Paper_Draft_Menu_of_cost-effective_interventions_for_mental_health.pdf?ua=1 (Accessed: 8 August 2020).
WHO (2020a) Adolescent Mental Health. Available at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed: 8th December 2020)
WHO (2020b) Depression. Available at: https://www.who.int/news-room/fact-sheets/detail/depression (Accessed: 8 August 2020).
WHO (2020c) The WHO mental health policy and service guidance package (2020). Available at: https://www.who.int/mental_health/policy/essentialpackage1/en/ (Accessed: 31 December 2020).
WHO | African Region (n.d.-c). Available at: https://www.who.int/choice/demography/african_region/en/ (Accessed: 8 August 2020).
WHO and Calouste Gulbenkian Foundation (2014) ‘WHO | Social determinants of mental health’. World Health Organization. Available at: http://www.who.int/mental_health/publications/gulbenkian_paper_social_determinants_of_mental_health/en/ (Accessed: 8 August 2020).
WHO | ATLAS 2010: First global report on substance use disorders launched (2010). Available at: https://www.who.int/substance_abuse/publications/Media/en/ (Accessed: 2 April 2020).
‘WHO | ATLAS Country Resources for Neurological Disorders’ (2017) WHO. World Health Organization.
WHO | Child and adolescent mental health (n.d.-a). Available at: https://www.who.int/mental_health/maternal-child/child_adolescent/en/ (Accessed: 8 August 2020).
WHO | South-East Asian Region (n.d.-d). Available at: https://www.who.int/choice/demography/seasian_region/en/ (Accessed: 8 August 2020).
WHO | The Mental Health Atlas 2017 (2017). Available at: https://apps.who.int/iris/bitstream/handle/10665/272735/9789241514019-eng.pdf (Accessed: 2 April 2020).
Wiley-Exley, E. (2007) ‘Evaluations of community mental healthcare in low- and middle-income countries: A 10-year review of the literature’, Social Science and Medicine. Pergamon, 64(6), pp. 1231–1241. doi: 10.1016/j.socscimed.2006.11.009.
Wolpert, M. (2020) Funders agree first common metrics for mental health science . Available at: https://www.linkedin.com/pulse/funders-agree-first-common-metrics-mental-health-science-wolpert/ (Accessed: 8 December 2020).
World Health Assembly, 65. (2012). Global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level: report by the Secretariat. World Health Organization. https://apps.who.int/iris/handle/10665/78898
World Health Organization, United Nations Children’s Fund, World Bank Group. Nurturing care for early childhood development: a framework for helping children survive and thrive to transform health and human potential. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO.
Yang, L., Thornicroft, G., Alvarado, R., Vega, E., Link, B. J., Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing ‘what matters most’ to identify culture-specific aspects of stigma, International Journal of Epidemiology, Volume 43, Issue 2, April 2014, Pages 494–510, https://doi.org/10.1093/ije/dyu039
Yaro, P. B. et al. (2020) ‘Stakeholders’ perspectives about the impact of training and sensitization of traditional and spiritual healers on mental health and illness: A qualitative evaluation in Ghana’, International Journal of Social Psychiatry. SAGE Publications Ltd, 66(5), pp. 476–484. doi: 10.1177/0020764020918284.
Zhong, H. et al. (2020) ‘Health outcomes and cost-effectiveness of treating depression in people with HIV in Sub-Saharan Africa: a model-based analysis’, AIDS Care – Psychological and Socio-Medical Aspects of AIDS/HIV. Routledge. doi: 10.1080/09540121.2020.1719966.
Appendix A: Disability weights used for mental health disorders in the GBD
| Disorder | Disability Weight |
| Anxiety disorders: mild | 0.03 |
| Anxiety disorders: moderate | 0.149 |
| Anxiety disorders: severe | 0.523 |
| Major depressive disorder: mild episode | 0.159 |
| Major depressive disorder: moderate episode | 0.406 |
| Major depressive disorder: severe episode | 0.655 |
| Bipolar disorder: manic episode | 0.48 |
| Bipolar disorder: residual state | 0.035 |
| Schizophrenia: acute state | 0.756 |
| Schizophrenia: residual state | 0.576 |
Note: Disability weights used in GBD (IHME, 2010)
